How Sustainable is Kidney Transplantation in a Pediatric Urology Practice: A Single Surgeon Experience
Jad A. Degheili, M.D.1, Michael E. Chua, M.D.2, Jin K. Kim, M.D.2, Jessica M. Ming, M.D.3, Walid A. Farhat, M.D., FRCS(C), FACS, GPLLM2.
1Division of Urology, Department of Surgery, American University of Beirut-Medical Center, Beirut, Lebanon, 2Division of Urology, The Hospital for Sick Children, Toronto, ON, Canada, 3Division of Urology, University of New Mexico, Albuquerque, NM, USA.
BACKGROUND:
Though the majority of pediatric renal transplants (PRT) are currently performed by dedicated transplant teams, there are few centers in North America where Urology is the primary surgical service. Herein we describe the outcomes of PRT performed by a single surgeon, and develop a learning curve model to achieve competence for this procedure.
METHODS:
We did a retrospective analysis of PRT cases performed by a pediatric urologist in the first 15 years of his practice immediately after fellowship training, where he had his first exposure to transplant surgery. Patients’ demographic, surgical data and outcomes were collected. Any associated surgical complications within 30-days post-op were evaluated as the primary outcome. The case characteristics, peri-operative data, and surgical outcomes were compared to cases performed by a senior surgeon who was considered the benchmark for comparison. To generate a learning curve plot, a cumulative sum analysis was performed to evaluate the evolution of practice in terms of operative time and surgical complication. We further assessed the differences between outcome and case characteristic differences after reaching the peak in learning curve.
RESULTS:
A total of 324 transplants were performed by 8 pediatric urologists between 2000 and 2015. A total of 55 (17%) were performed by the surgeon under evaluation, while 78 (24%) were performed by the senior pediatric urologist. Patients’ characteristics revealed significant differences between donor type (senior surgeon performing more living donors; p<0.0001), and the index surgeon incorporating uretero-ureteral anastomoses into his practice (p=0.001). Both operative time and ischemia time were noted to be statistically significant between the index and senior surgeon (226 vs. 252min, p=0.006 and 40 vs. 30min, p=0.001; respectively); while the 30-day surgical complication rates were not significantly different between the two surgeons (18 (32.7%) versus 28 (35.9%), p=0.853 for the index and senior surgeons; respectively). Further differential cluster analysis according to the case characteristic differences, the overall operative time was not significantly different; while the warm ischemia time was only significantly longer for the index surgeon specifically among deceased donor cases (p= 0.007). The cumulative sum analysis for the 55 performed cases, generated a learning curve of which maximal complication rates and operative times did not increase beyond the 17th case performed which occurred at the 5th year into the analysis (Figure 1). While comparing the cases characteristics and perioperative outcomes after the peak of the learning curve, only warm ischemia time was significantly different (p=0.003).
CONCLUSION:
If incorporating this into a pediatric urologist’s practice, a primary focus should be on performing these cases within the first few years of his or her career to solidify operative skills and achieve optimal outcomes. Even though, technically, a surgeon may have the skills at 17 transplants, a dedicated team with a primary surgeon, whether it be a pediatric urologist or transplant surgeon, who maintains proficiency in the operation should be the main provider for these children. 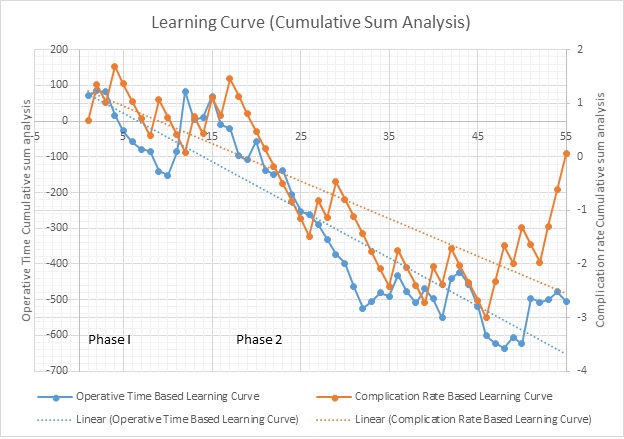
Back to 2018 Program




