Standardization of care for bladder exstrophy: Development of an evidence and best-practice based protocol for neonatal, pre-operative and post-operative care
Courtney K. Rowe, MD, Jean Dearn, RN, Paul A. Merguerian, MD, MS.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: With the success of standardized clinical pathways in streamlining care for common medical conditions, attention has been turned to more complex conditions. We describe our institution’s experience creating an evidence and guideline-based pathway for care of patients with classic bladder exstrophy, from neonatal diagnosis through pre-operative workup to post-operative care. We hypothesize that standardized care will improve safety, quality, delivery of care, engagement of medical professionals, family satisfaction and costs.
METHODS: A multi-disciplinary clinical working group was formed as a collaboration between pediatric urology, orthopedic surgery, anesthesiology and pain medicine, infectious disease, nursing and social work. We used our institution’s clinical standard work pathway process for quality improvement. A literature search was performed in Ovid Medline, Cochrane Database of Systematic Reviews, Embase, National Guideline Clearinghouse and TRIP. We evaluated the evidence regarding bladder exstrophy surgical approach, method of pelvic fixation, use of prophylactic antibiotics, intra-operative transfusion goals, optimal postoperative pain control and use of postoperative anticholinergics. 777 records were screened, 193 records were assessed and 15 papers were graded and included in pathway development. Due to the paucity of evidence in some areas, an informal survey regarding management of classic bladder exstrophy was sent to and high volume bladder exstrophy centers.
RESULTS: The multi-disciplinary group developed an evidence and best-practice based protocol spanning prenatal diagnosis, neonatal admission, pre-operative workup, intra-operative management and post-operative care. Order sets were created for neonatal and post-operative admissions as well as outpatient clinic visits. Family education documents were created in conjunction with nursing staff and patient education. Enrolled patients will be tracked prospectively for neonatal and postoperative length of stay, postoperative complications and readmissions for their first 2 years of life. The pathway itself is publically available on our institution’s external website and can be accesses by pediatricians, obstetricians, referring physicians and outside pediatric urologists.
CONCLUSIONS: Care for complex conditions can be standardized through evidence based clinical pathways and in the absence of evidence, best practices can be developed with national input and local consensus. Evidence-based choices allow for efficient care delivery. Standardized timelines help families and caregivers understand what to expect in the child’s first year of life. Having all patients on a pathway will allow outcomes to be tracked with less variation in care. With time, this may translate to improved outcomes including decreased length of stay, decreased readmissions and improved family experience due to clear education and expectations for care. 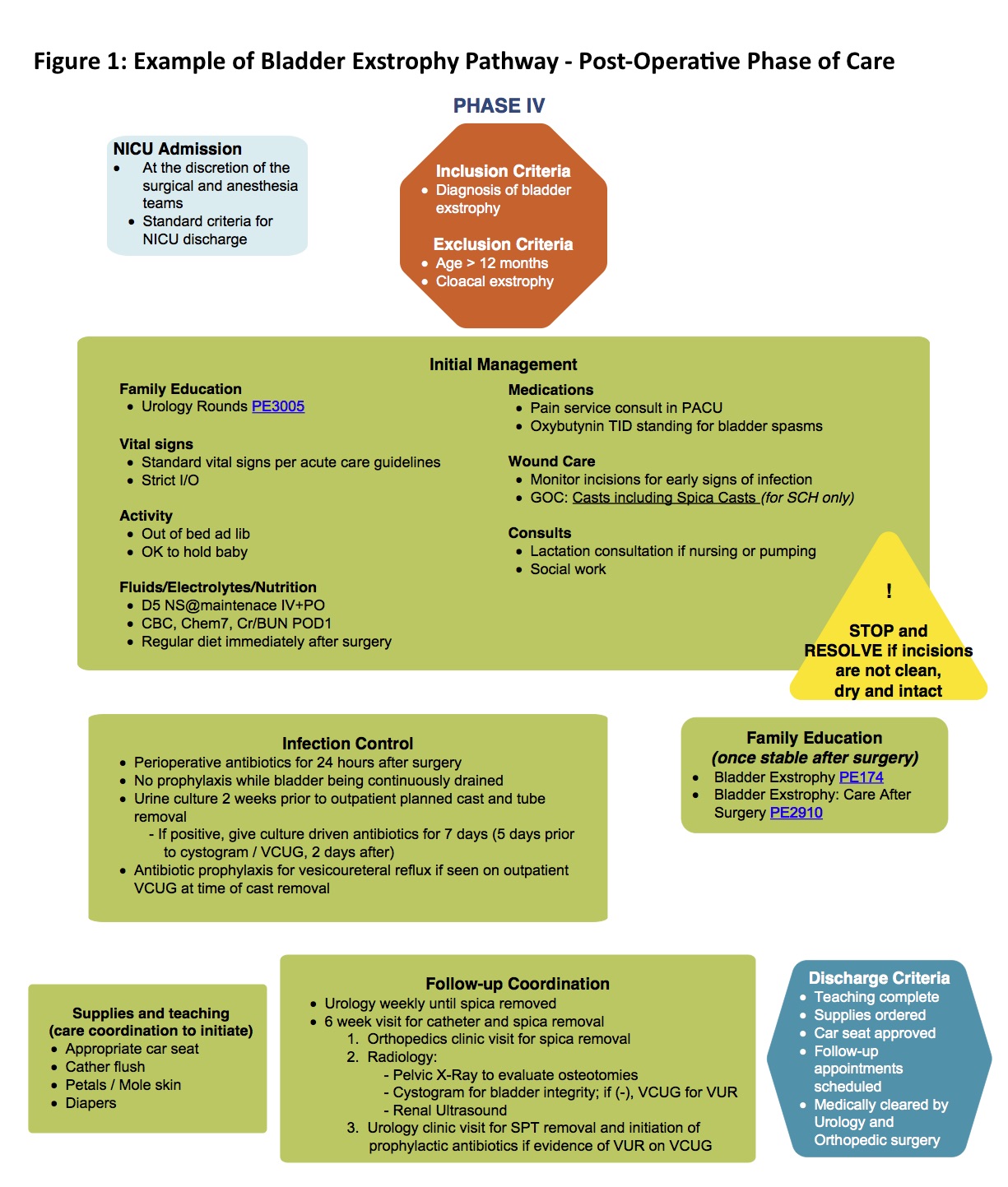
Back to 2018 Program




