Long-Term Clinical Outcomes and Parental Satisfaction After Dextranomer/Hyaluronic Acid Injection for Primary Vesicoureteral Reflux
Michelle A. Lightfoot, MD, Aylin N. Bilgutay, MD, Noah Tollin, BA, Scott Eisenberg, BA, Jake Weiser, BA, Edwin Smith, MD, James Elmore, MD, Hal Scherz, MD, Andrew J. Kirsch, MD.
Children's Healthcare of Atlanta, Atlanta, GA, USA.
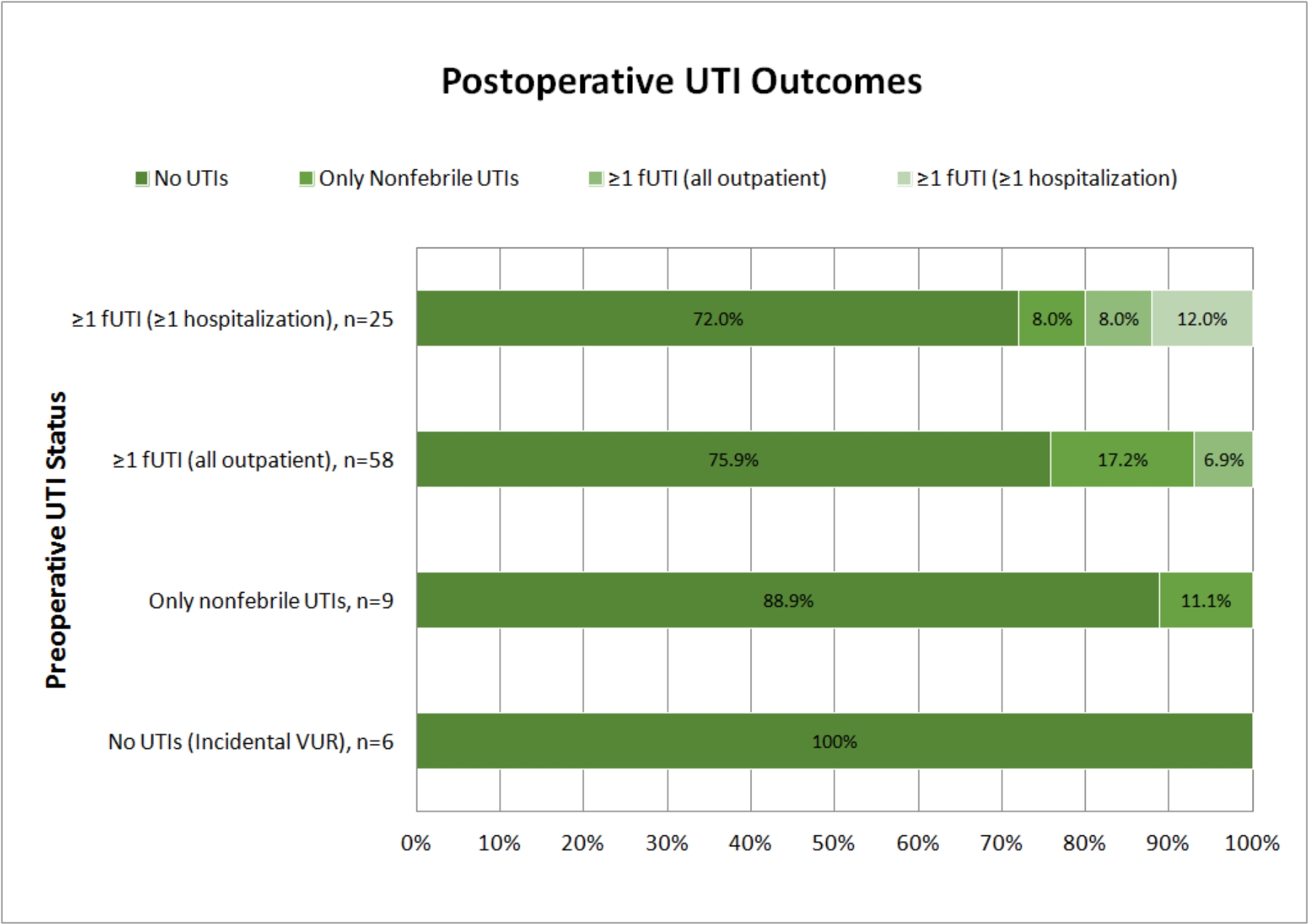
Background: Endoscopic injection with dextranomer/hyaluronic acid (Dx/HA) is a common treatment for vesicoureteral reflux (VUR) with short-intermediate term success rates >90% in our experience. However, long-term outcomes and parental opinion of Dx/HA injection are not as well-established. We assessed both long-term outcomes and degree of parental satisfaction for patients undergoing Dx/HA injection for primary VUR with >5 year follow-up. Methods: After IRB approval, the families of all patients having Dx/HA injection for primary VUR at our institution between 2008 and 2012 were called for the purpose of conducting a telephone interview. The medical records of those patients whose parent completed the interview were then reviewed. Data collected by phone interview included degree of parental satisfaction (highly satisfied, partially satisfied, and dissatisfied) and reasons given for response, as well as presence of UTIs before and after surgery. Chart review data included patient demographics, radiographic VUR data, need for secondary surgery, and surgical indications. Results: 575 patients were identified who had Dx/HA injection for primary VUR between 2008 and 2012. Of these patients, the parents of 99 (17%) were successfully contacted and participated in the telephone interview. Median follow-up time from surgery to phone survey was 8.4 years (IQR 6.8-9.6 years). Secondary surgery was performed in 13/99 (13.1%) patients. Seven patients (7.1%) underwent secondary Dx/HA injection for persistent VUR without UTIs at a median of 0.35 years postoperatively (IQR 0.33-0.77 years). Five patients (5.1%) underwent Dx/HA injection (n=3) or ureteral reimplantation (n=2) for VUR with febrile UTIs (fUTIs) at a median of 2.2 years (IQR 1.3-5.1 years), and 1 patient (1.0%) had a ureteral reimplantation for symptomatic obstruction 2.8 years after initial surgery. Of the 13 patients who underwent secondary surgery, 4 (30.8%) had additional surgery for VUR with fUTIs (n=3) or unknown indications at a different facility (n=1). Of the 83/98 (84.7%) of families who reported ≥1 fUTI prior to surgery, only 9/83 (10.8%) reported any fUTIs after surgery (clinical success 89.2%). No patient without a reported fUTI before surgery developed a fUTI after surgery. Clinical success (no fUTIs after surgery) was 93.1% in patients who had only outpatient preoperative fUTIs and 80% in those who were hospitalized at least once for treatment of a fUTI before surgery (Figure). Parental satisfaction with the procedure was high, with a 94.1% satisfaction rate, 2.4% partially satisfied, and 3.5% dissatisfied. Reasons for partial satisfaction consisted of recurrent UTIs (n=2), and reasons for dissatisfaction included persistent VUR requiring multiple operations (n=1) and failure to cure VUR in patients with incidental diagnoses and no UTIs before or after surgery (n=2). Conclusions: Endoscopic injection with Dx/HA for primary VUR has a very good long-term success rate and high parental satisfaction. Postoperative ureteral obstruction is rare but may occur years after the initial procedure justifying initial sonographic surveillance and repeat imaging in symptomatic patients.
Back to 2018 Program




