Psychiatric Disease in Patients with Complex Congenital Urologic Anomalies
Claire M. de la Calle, MD, Thomas W. Gaither, MD, Hillary L. Copp, MD.
UCSF, San Francisco, CA, USA.
Background:
Patients with complex congenital urologic anomalies are now living longer and adults with chronic disease are at risk for mental health issues such as depression. Little information exists on psychiatric disease burden among patients with complex congenital urologic anomalies.
Methods:We used of the Office of Statewide Health Planning and Development (OSHPD), which captures all the hospital discharges in California to identify patients with common congenital urologic anomalies (bladder exstrophy, posterior urethral valves (PUV), prune belly syndrome (PBS), epispadias, spina bifida and disorders of sexual development (DSD)). Among patients with complex congenital urologic anomalies we assessed admissions for mental health issues from 1990 to 2014 using ICD-9 codes 291 – 305, 307 – 309, 311 – 314 as the primary diagnosis for admission. Differences between groups were compared with chi-square or student t-test as appropriate. Logistic modeling was used to identify predictors of mental health admissions among patients with complex congenital urologic anomalies, controlling for age, sex, race, urban versus rural home location, private versus non-private payer category, length of stay and type of congenital anomaly.
Results:
We identified 87,112 hospital discharges from 1990 to 2014 for patients with congenital urologic anomalies, and 1,489 (1.71%) of those discharges were for primary mental health issues. The number of admissions for mental health issues have increased by 4-fold from 1990 to 2014 (Figure 1). Patients admitted for mental health issues were older (mean age 34.2 years, SD 14.3) compared with those admitted for non-mental health admissions (mean age 20.5 years, SD 19.9). Males were less likely to be admitted for mental health issues; six hundred and twenty (41.6%) of the admissions for primary mental health issues were male patients versus 42,449 (49.6%) for the admissions for non-primary mental health issues (p <0.001). Spina bifida was the most common urologic congenital anomaly in the cohort (79.7%). In a multivariate analysis predictors of mental health admissions were age (OR 1.02, CI 1.01 – 1.02) and female gender (OR 1.15, CI 1.01 – 1.30). The congenital anomalies at highest risk for admission were DSD (OR 8.78, CI 3.58 – 21.5), spina bifida (OR 5.85, CI 2.42 – 14.2), and prune belly (OR 2.96, CI 1.04 – 8.44). Overall the top admissions for mental health issues were for mood disorders (includes bipolar disorders, manic affective disorders and major depressive disorders and depression NOS (not otherwise specified)), followed by schizophrenia and other non-organic psychoses, followed drug and alcohol abuse related mental disorders.
Conclusions:Patients with complex congenital urologic anomalies can suffer from mental health issues, especially during their adult life. A significant increase in hospitalizations for mental health issues among patients with complex congenital urologic anomalies, occurred in California between 1990 and 2014. Further investigation is necessary to better understand how to provide improved care for this population.
Figure 1: Mental health admissions among patients with complex congenital urologic anomalies 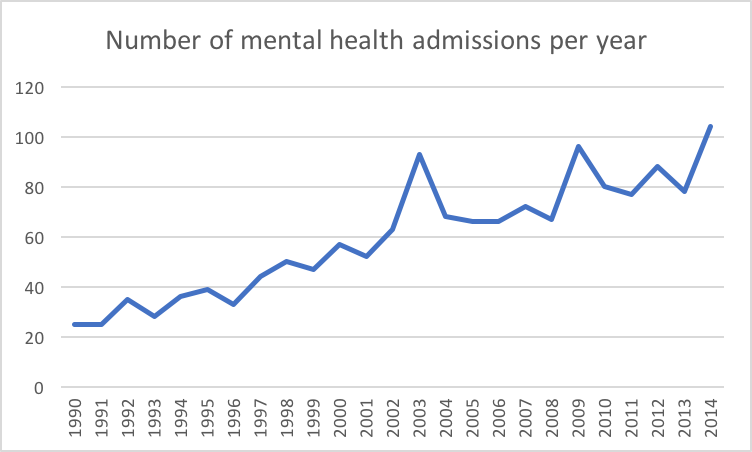
Back to 2018 Program




