Quantitative Characterization of Renal Parenchymal Scarring on Ultrasound
Jennifer E. Reifsnyder, MD1, Sleiman R. Ghorayab, PhD2, Preeya K. Mistry, MD1, Stella Glykos, BS3, Lane S. Palmer, MD4.
1Division of Pediatric Urology, Cohen Children's Medical Center, Northwell Health, New Hyde Park, NY, USA, 2School of Engineering and Applied Sciences, Ultrasound Research Laboratory, Hofstra University & Radiology and Molecular Medicine, Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY, USA, 3School of Engineering and Applied Sciences, Ultrasound Research Laboratory, Hofstra University, Hempstead, NY, USA, 4Division of Pediatric Urology, Cohen Children's Medical Center, Northwell Health & Zucker School of Medicine at Hofstra/Northwell, New Hyde Park, NY, USA.
BACKGROUND: Dimercaptosuccinic acid (DMSA) scan is the gold standard for identifying renal scarring following infection as sonography requires large areas of scarring to be recognized. The well-known benefits of sonography include absence of radiation exposure, noninvasive quality, rapid acquisition, and ease of availability. Identifying subtle sonographic differences in potentially scarred renal parenchyma would positively impact care. We previously used heterogeneity index (HI) to identify differences between normal and diseased renal parenchyma (obstruction, hypertension). This study sought to compare the heterogeneity of renal parenchyma in areas of known scarring to areas without scarring, and to normal kidneys, in order to develop a noninvasive method to identify areas of potential renal scarring using ultrasound alone. METHODS: We reviewed DMSA scans for the presence of scarring in children imaged at least 12 weeks following a febrile urinary tract infection (UTI) or for congenital dysplasia and compared their corresponding ultrasounds. A group of normal controls was included; all controls underwent abdominal ultrasound imaging for reasons unrelated to the urinary tract. Multiple sagittal images of each kidney were collected, and multiple regions of interest (ROIs) within the renal parenchyma were analyzed by a technique that converts pixels from gray-scale images into a binary map to generate a heterogeneity index (HI). Descriptive statistics and independent samples T-tests were used to compare heterogeneity in kidneys of pediatric patients with known renal scarring to those with normal kidneys. RESULTS: Among the 18 subjects who underwent DMSA scan to evaluate for renal scarring, 12 (67%) were female and 6 (33%) were male. All thirteen (72.2%) patients with evidence of renal scarring on DMSA scan had a history of UTI. Eight normal controls without history of UTI were included. Within the cohort of normal controls as well as among patients with a normal DMSA scan (no scarring), the median HI for both groups was 1.4. The median HI for patients with diffuse renal scarring was 1.6, which was significantly higher than the normal control kidneys (p<0.002). In patients with focal renal scarring present in the upper pole, the median HI of the regions corresponding to the areas of scarring was 1.6 (upper pole) and 1.8 (midpole); both values are significantly higher than the normal controls (p<0.00005, Table). CONCLUSIONS: Heterogeneity on renal sonogram was significantly higher in regions corresponding to areas of scarring identified on DMSA scan. Quantification of parenchymal heterogeneity provides a novel way to assess renal parenchymal damage in children. 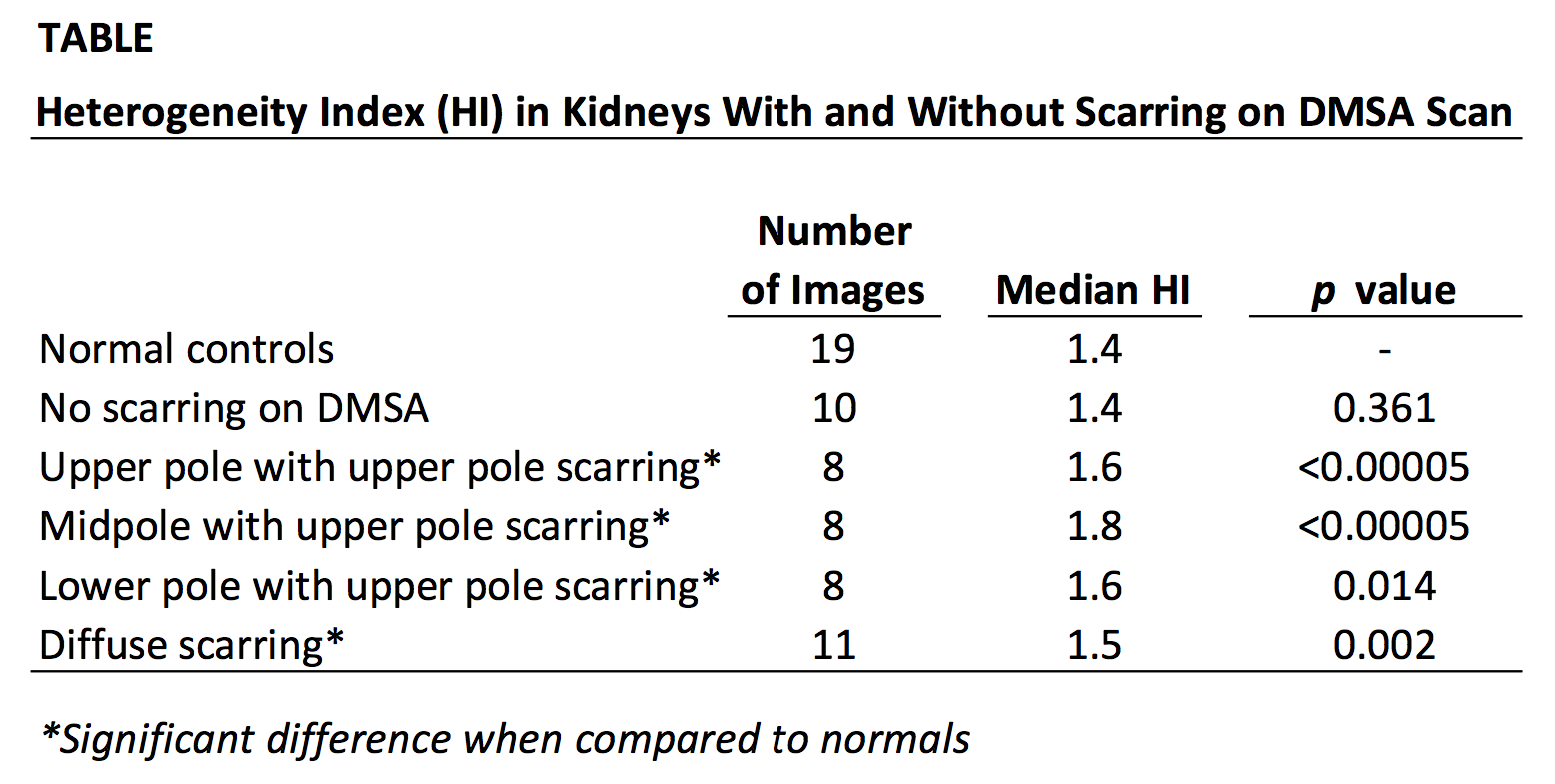
Back to 2019 Abstracts




