To Stage or Not to Stage: Surgeon Intuition and Early Complications in Proximal Hypospadias Repair
Anthony D'Oro, BA, Yvonne Y. Chan, MD, Ilina Rosoklija, MPH, Emilie K. Johnson, MD, David I. Chu, MD, Bruce W. Lindgren, MD, Dennis B. Liu, MD, Edward M. Gong, MD, Max Maizels, MD, Theresa Mayer, MS, RN, Earl Y. Cheng, MD, Elizabeth B. Yerkes, MD.
Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA.
BACKGROUND: Many factors influence surgeons' decisions to pursue single or multi-stage repairs for proximal hypospadias (PH), but there is limited data to indicate what these factors are and how such decisions affect outcome. This study aims to identify patient characteristics which contributed to surgeons' staging decisions for PH repair and to identify early surgical outcomes. We hypothesized that patients with more atypical genital features, narrower glans and urethral plates, higher ratio of post- to pre-degloving penile length, and longer urethroplasty length would be more likely to undergo staged repair. Additionally, we hypothesized that patients selected for single-stage repair would have higher rates of post-operative complications and unplanned surgeries.
METHODS: Patients from a single-center who underwent primary hypospadias repair between 07/2011-03/2018 were identified from a prospective database with intra-operative measurements. Patients with PH noted prior to or after penile degloving were included. Patients without intra-operative measurements were excluded. Patients were placed into two groups (single-stage or multi-stage) based on the surgeons' final intra-operative staging decision. Clinical characteristics, intra-operative penile measurements, rates of post-operative complications, and unplanned surgeries were compared between groups using Fisher's exact and Mann-Whitney U tests.
RESULTS: 111 patients met inclusion criteria, including 50 in the single-stage group and 61 in the multi-stage group. Compared to those in the single-stage group, patients in the multi-stage group had higher rates of meatal location proximal to the penoscrotal junction (31/61, 51% vs. 5/50, 10%; p<0.001), chordee >60º (53/61, 87% vs 20/47, 43%; p<0.001), penoscrotal transposition (31/61, 51% vs 4/50, 8%; p<0.001), bifid scrotum (34/61, 56% vs 8/50, 16%; p<0.001), undescended testes (14/61, 23% vs 4/50, 8%; p=0.04) (Table 1). Additionally, patients who underwent multi-stage repair had narrower median glans width (13.5mm [range: 7-20] vs 15mm [range: 8-19]; p=0.01) and longer median length of urethroplasty (38mm [range: 18-70] vs 18mm [range: 7-35]; p<0.001) compared to patients who underwent single-stage repair (Table 2). There were no significant differences between groups for shaft urethral plate width (3mm [range: 1-12] vs 4mm [range: 1-10]; p=0.07) and ratio of post- to pre-degloving non-stretched penile length (1.6 [range: 1-3] vs. 1.5 [range: 1.1-2.6]; p=0.50). After a median 18.2 months of follow-up (range: 0.1-70.8), patients who underwent single-stage repair had higher rates of post-operative complications (29/50, 58% vs. 23/61, 38%; p=0.04) and unplanned surgeries (23/50, 46% vs. 18/61, 30%; p=0.08) than those with planned multi-stage repairs.
CONCLUSION: In this study, surgeons elected multi-stage repair of PH for patients with more atypical genital features. Despite having more favorable characteristics, patients selected for single-stage repairs had >50% complication rate at early follow-up. Although there may be fine points of decision-making not identified here, the data suggests that intuition may be misleading and staged repair should be considered more commonly. 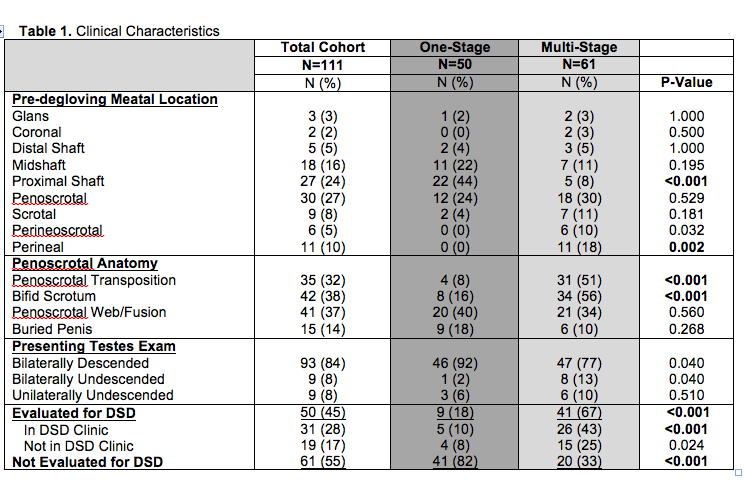

Back to 2019 Abstracts




