The Pudendal Nerve Block for Ambulatory Urology: The Old Is New Again
Thomas S. Lendvay, MD1, Henry Huang, MD1, Chinonyerem Okoro, MD2, Daniel Low, MD1.
1Seattle Children's Hospital, Seattle, WA, USA, 2University of Washington, Seattle, WA, USA.
BACKGROUND: Caudal epidural analgesia (CEA) is a common analgesic technique performed for pediatric penile surgeries. Recent evidence has implicated an association between hypospadias fistulas and CEA. Additional risks of CEA include epidural related complications, motor blockade, urinary retention, and is contraindicated in children with lower back abnormalities or coagulopathy. The pudendal nerve block (PNB) is an effective analgesic alternative to CEA and lasts up to 12 hours post-injection. We demonstrate our initial experience employing PNB for ambulatory pediatric urology procedures.
METHODS: Using retrospective, non-randomized, time-series, observational real world data, a comparative effectiveness study of CEA and PNB was performed. Patients less than five years old, who underwent circumcision, hypospadias repair, congenital chordee repair, correction of penile angulation, buried penis repair with or without scrotoplasty, meatotomy, or lysis of penile adhesions between June 1, 2016 - December 31, 2018 for CEA and between January 1, 2018 - May 15, 2019 for PNB in an Ambulatory Surgery Center at a single institution were included. Post Anesthesia Care Unit (PACU) pain scores, anesthesia prep time (minutes), morphine rescue rates in PACU, emergence time (end of surgery to out of room - minutes), and length of recovery room stay (minutes) were determined. All PNBs were performed with 0.2% - 0.5% Ropivacaine (0.2-0.3 mL/kg) and all CEAs were performed with 0.2% Ropivacaine (0.5 - 1 mL/kg).
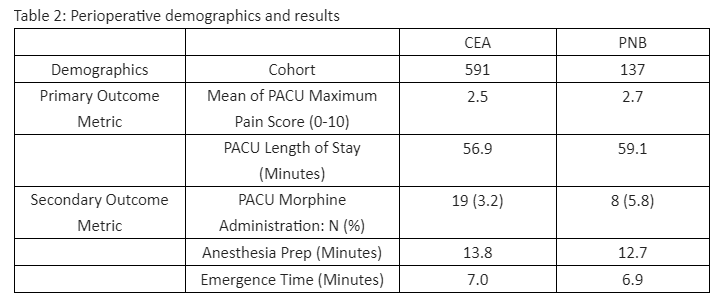
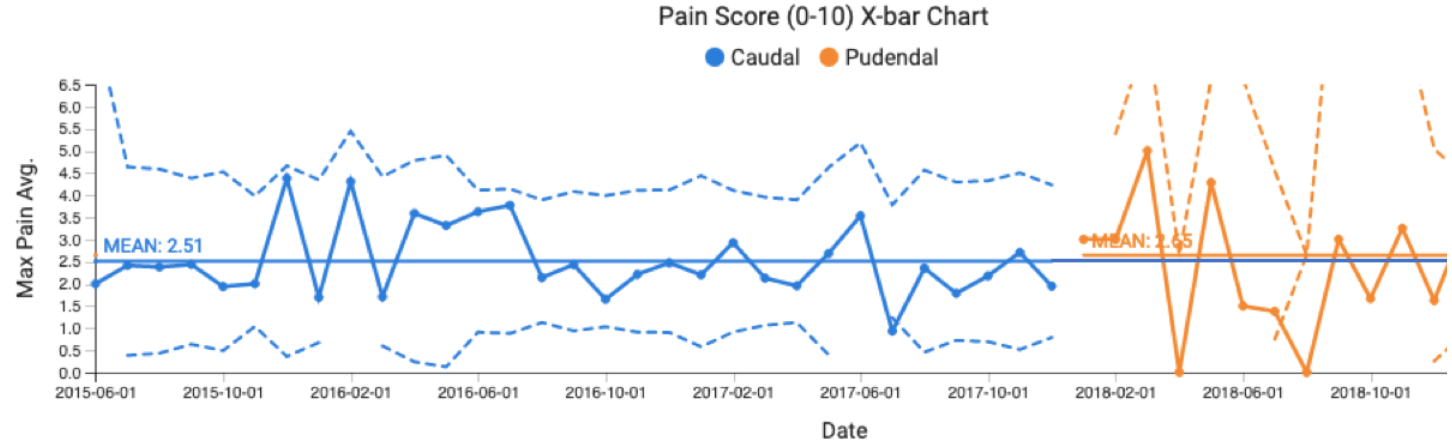
RESULTS:A total of 728 patients were identified; 591 and 137 received CEA and PNB, respectively. PNB were done using ultrasound guidance. Demographic data was comparable between the two cohorts. Anesthetic protocols are in Table 1. There was no special cause variation between CEA and PNB cohorts for pain score, 2.5 vs. 2.7 (Figure 1.); for anesthesia prep time 13.8 min vs. 12.7 min; for morphine rescue rates, 3.2% vs. 5.8%; emergence time, 7.0 min vs. 6.9 min; and PACU length of stay, 56.9 min vs. 59.1 min. (Table 2).
CONCLUSIONS: For pediatric penile surgeries, ultrasound-guided PNB is as effective as CEA. The simplicity and safety of the PNB as well as the equivalent results of our observational study warrants further prospective investigation and may reduce potential morbidity from caudal anesthesia. 
Back to 2019 Abstracts




