Predictors of Nephrectomy after High Grade Renal Trauma: An Assessment of the National Trauma Data Bank (NTDB)
Ching Man Carmen Tong, DO1, Kendrick Campbell, BA2, Hannah Phelps, MD2, Shilin Zhao, PhD3, Harold N. Lovvorn, III, MD4, Abby S. Taylor, MD1, Stacy T. Tanaka, MD1, John W. Brock, III, MD1, Mark C. Adams, MD1, John C. Pope, IV, MD1, John C. Thomas, MD1, Chevis Shannon, MBA, MPH, DrPH5, Douglass B. Clayton, MD1.
1Division of Pediatric Urology, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, USA, 2School of Medicine, Vanderbilt University, Nashville, TN, USA, 3Department of Biostatistics, Vanderbilt University, Nashville, TN, USA, 4Department of Pediatric Surgery, Monroe Carell Jr. Children's Hospital at Vanderbilt, Nashville, TN, USA, 5Department of Neurosurgery, Vanderbilt University Medical Center, Nashville, TN, USA.
Introduction
The management of pediatric renal trauma currently follows adult trauma guidelines. While efforts have been made to determine which patients with high-grade renal trauma can be treated conservatively, the national trends and predictors of nephrectomy in these patients remain unclear. Thus, we used the National Trauma Data Bank (NTDB) to address such questions. We hypothesized that injury mechanism, patient age and adult hospital care are independent predictors of nephrectomy as compared to endoscopic management for patients with high-grade renal trauma.
Methods
We acquired patient data from NTDB (2010-2015), the largest multi-center trauma repository with injury specifics and outcomes from all geographic regions. In our analysis, we included patients younger than 18 years old with renal injuries using the Abbreviated Injury Score (AIS) code. We defined high grade renal trauma as grade III or higher using the American Association for the Surgery of Trauma (AAST) grading system. Injury mechanism, AAST grade, patient demographics, hospital course and complications were recorded. Unadjusted and adjusted statistical analyses were performed using R statistical software including both univariate and multivariate analysis to assess the primary outcome, predictors of nephrectomy.
Results
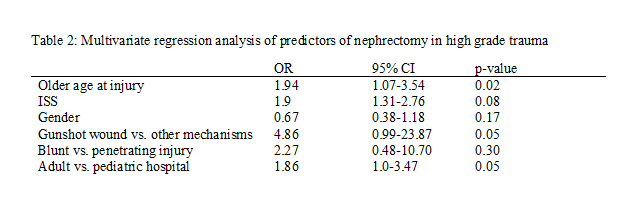
We identified 6469 subjects in NTDB who sustained renal trauma, of which 3924 (61%) were considered AAST grade III or higher. We found that 689 (24%) patients in the dataset received care at an academic adult trauma level I or II hospital while 2215 (76%) patients received care at a pediatric institution. Of the patients with high grade trauma, we identified 263 patients who underwent endoscopy and 263 who underwent nephrectomy with complete data necessary for univariate and multivariate analyses. When considering patients undergoing surgery, more patients underwent endoscopic intervention at pediatric hospitals (8% vs. 5%, p=0.008) while more patients receiving care at an adult hospital underwent nephrectomy (8% vs. 5%, p=0.013). On univariate analysis, multiple factors including age, gender, injury severity score (ISS), type and mechanism of injury, as well as treatment at an adult hospital, were significantly associated with nephrectomy compared to endoscopic approach (table 1). However, multivariate regression analysis controlling for demographics and injury characteristics revealed that age, gunshot wound and care at an adult hospital were the strongest independent predictors of nephrectomy in high grade renal injury (table 2).
Conclusion
Using the NTDB, we globally assessed national practice patterns of nephrectomy in high grade renal trauma. While age and gunshot wounds are not surprising predictors of nephrectomy, presentation at an adult hospital highlights the need for better understanding of the differences in assessment and management of renal trauma between adult and pediatric trauma centers. The execution of multi-institutional studies that analyze trauma characteristics, surgical outcomes and urologic consultation will help further delineate the utility of nephrectomy in this vulnerable population.

Back to 2019 Abstracts




