Impact of Trauma Center Designation in Pediatric Renal Trauma: Prospective National Trauma Data Bank analysis
Laura Bukavina, MD MPH1, Kirtishri Mishra, MD1, Mike Swindle, BS2, Vaishnavi Narayanamurthy, MS2, Melody Chen, MD1, Jonathan Ross, MD3, Lynn Woo, MD3.
1University Hospitals Cleveland Medical Center/ Case Western Reserve Medical University, Cleveland, OH, USA, 2Case Western Reserve Medical University, Cleveland, OH, USA, 3University Hospitals Cleveland Medical Center/ Rainbow Babies and Children's Hospital, Cleveland, OH, USA.
BACKGROUND: Pediatric renal trauma may be managed differently across different tier trauma centers in the United States. Our aim was to examine these differences in the management of renal trauma in pediatric population and assess differences in outcomes based on hospital trauma level designation across the United States
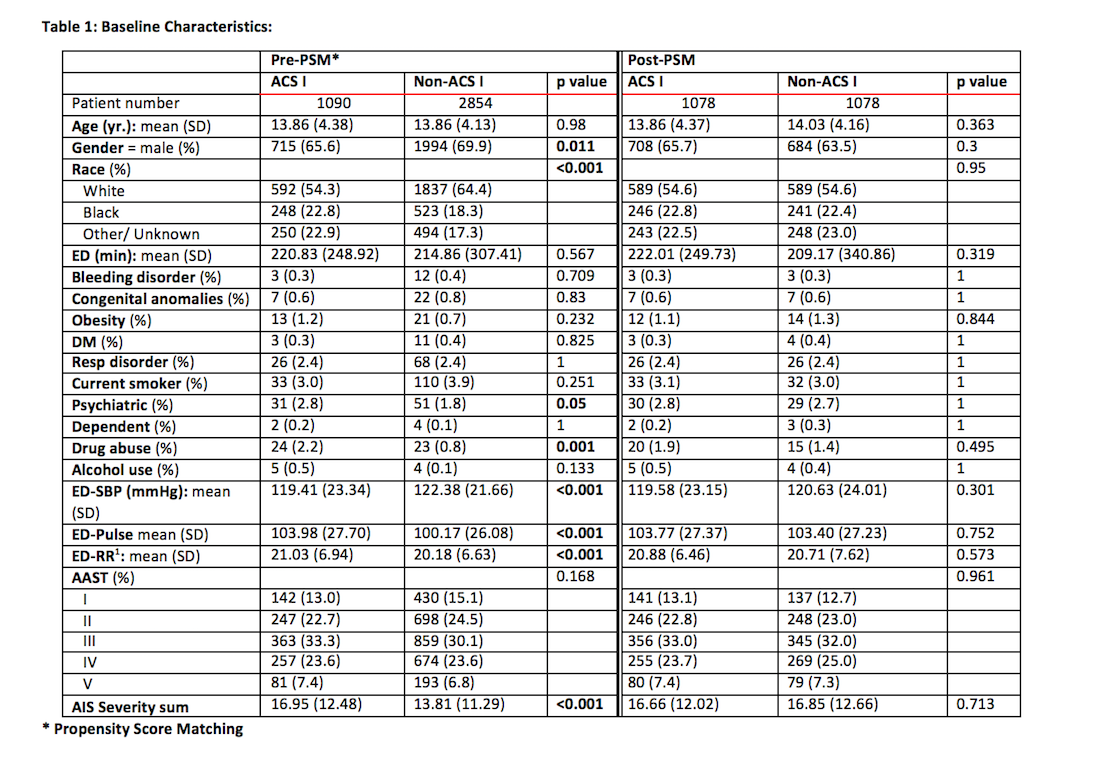
METHODS: We performed a review of the American College of Surgeons'(ACS) National Trauma Data Bank ( NTDB) database from 2011 to 2016. Renal injuries treated at ACS NTDB trauma centers from 2011 to 2016 in pediatric population ( 0-18) were identified. Propensity score matching (PSM) was utilized to adjust for baseline differences between level I and non level I cohorts. Patients were stratified according to initial management of renal injury into the 3 groups of 1) operative 2) minimally invasive procedure 3) conservative management (no active intervention). Univariate and multivariable logistic regression further compared odds of each above mentioned management outcome in patients in level I trauma vs non level I trauma center as well as identified risk factors for complications, transfusion, and intervention.
RESULTS: A total of 2,156 pediatric patients diagnosed with renal trauma between 2011 and 2016 were identified in NTDB with the target ICD-9 and AAST codes and included in the analysis after propensity score matching.. On univariate analysis, there were no differences in the rate of nephrectomies [ 24 (2.2) vs 14 (1.3), p=0.141], minimally invasive interventions [30 (2.8) vs 28 (2.6), p=0.894], or any operative intervention [26 (2.4) vs 14 (1.3), p=0.079]. Similarly, there was no difference in complications including UTI, DVT, surgical site infection, sepsis, or return to OR among the level I vs non level I trauma centers. When specifically looking at risk factors associated with intervention of any sort ( minimally invasive or operative), after adjusting for age, race, AAST, hospital tier, drug abuse, vitals, and individual hospital factors; hospital designation was not found to be predictive for more aggressive management. Factors associated with an intervention included higher grade injury AAST III ( OR 4.97), IV (21.466) and V (37.971) .
CONCLUSIONS: Pediatric renal trauma is similarly managed across all ACS tiered trauma centers, with rate of any operative intervention more prevalent in the high grade renal injuries. 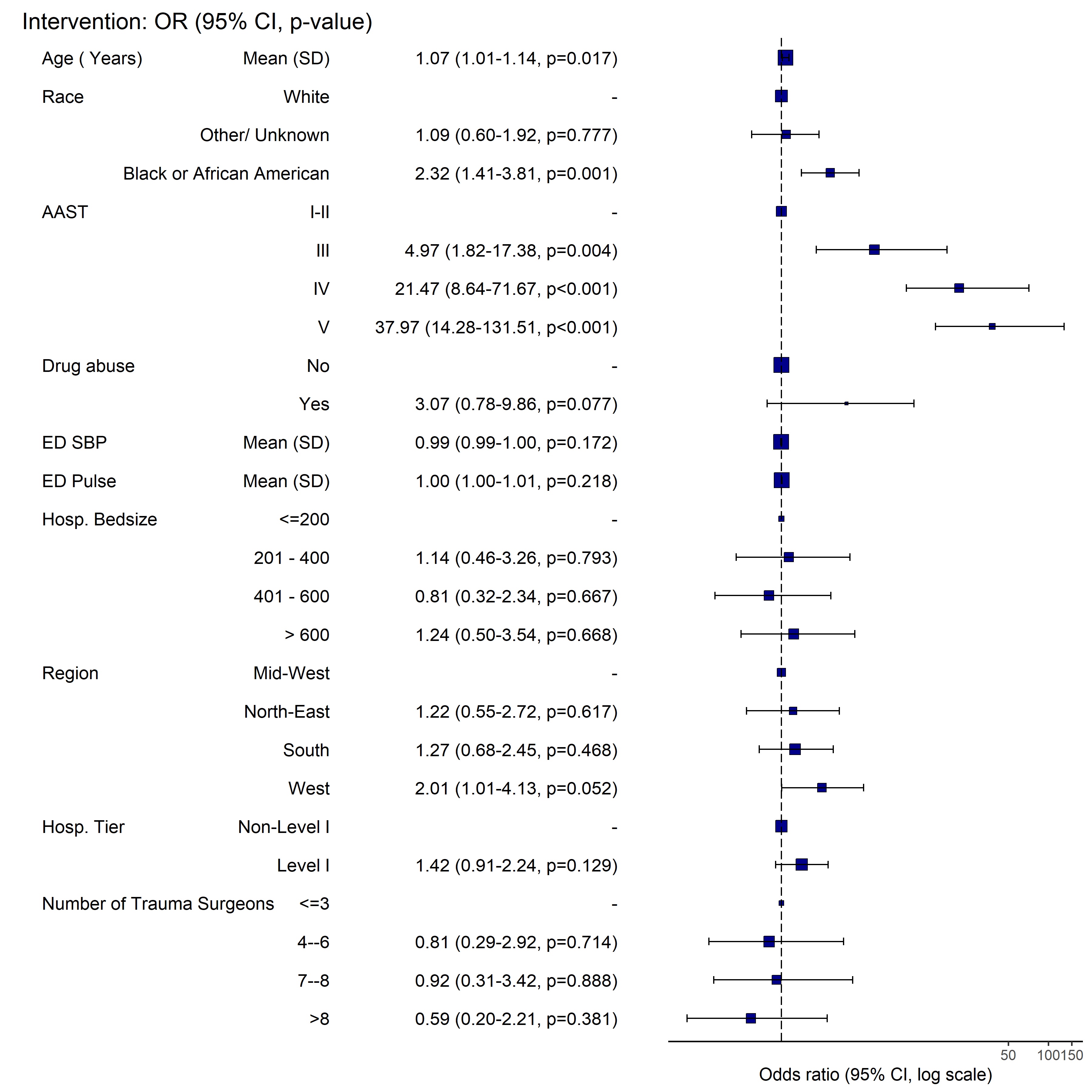
Back to 2019 Abstracts




