New-onset ESRD in adults secondary to reflux nephropathy has decreased in incidence since 1995
Laura B. Cornwell, MD1, Jonathan V. Riddell, MD2, Matthew D. Mason, MD2.
1Rady Children's Hospital, San Diego, CA, USA, 2SUNY Upstate Medical University, Syracuse, NY, USA.
BACKGROUND: Vesicoureteral reflux (VUR) and reflux nephropathy (RN) are well known entities in urology and nephrology, however their relationship remains incompletely understood. Management of VUR has become more conservative over time in the effort to minimize overtreatment. We sought to examine the impact of this change on the incidence of end stage renal disease (ESRD) due to RN. METHODS: The United States Renal Data System (USRDS) is a national data system that collects information about chronic kidney disease and ESRD. Since 1995, the USRDS has mandated that all dialysis centers enroll and submit data on new-onset ESRD patients. Of the over 2.5 million patients enrolled since 1995, 7505 were enrolled with a diagnosis code for RN as the primary cause of ESRD. We report the trends seen in this patient population from 1995 to 2015.
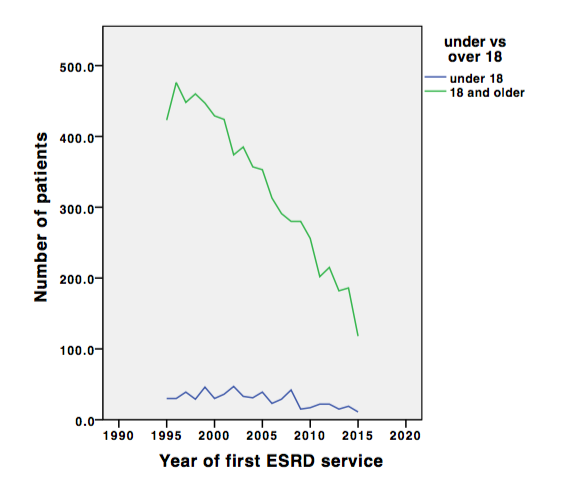
RESULTS:The absolute number of patients with new-onset ESRD attributed primarily to reflux nephropathy has seen a steady decrease over time, with a 2.5 fold difference between 1996 (506/year) and 2014 (205/year) (R2 = 0.942, p<0.001). Taking into account US population data, the incidence has decreased 3.2 fold from 1.9 to 0.6 per 1,000,000. 58.8% of the patients were female, 87.2% white. The mean age at the time of ESRD onset was 47 (IQR 30-65) and this did not significantly vary over the years (P>0.05). However, when comparing pediatric new-onset ESRD to adult-onset disease, a trend approaching significance (p=0.053) was seen with a decrease in incidence of adult ESRD but a relatively steady incidence of pediatric ESRD (mean age 12, incidence 15-47/year), see figure 1.
66.8% of patients were also hypertensive, 5.3% with diabetes, and 5.9% had no known comorbidities. Over the period, new patients with ESRD were more likely to be hypertensive and less likely to have diabetes (p<0.001). 73.4% did not need dialysis at the time of ESRD diagnosis, likely related to the finding that most patients were followed by a surgeon (74.0%) for over 12 months (59.7%). 44.5% of patients received transplantation at a mean age of 35 years old, 18.4 months (IQR 5-39) after ESRD diagnosis. 55.6% of patients in the dataset had died at a mean age of 62 (IQR 50-76), 60 months (IQR 16-90) after ESRD diagnosis.
CONCLUSIONS: Adult-onset ESRD attributed to RN has decreased in incidence over the decades, possibly as a result of urological care for VUR. The lack of a corresponding trend in the pediatric ESRD population suggests that severe disease in younger patients may be innately irreversible.
Back to 2019 Abstracts




