Higher prevalence of benign tumors in men with testicular tumors and history of treated cryptorchidism
Rachel Davis, MD, Mahir Maruf, MD, Joseph Cheaib, MD, Phillip Pierorazio, MD, Heather Di Carlo, MD.
Johns Hopkins School of Medicine, Baltimore, MD, USA.
BACKGROUND: Cryptorchidism or undescended testis (UDT) is a known risk factor for testicular cancer, increasing the risk for testicular cancer almost 6-fold if untreated and almost 2-3-fold if surgically corrected before puberty. Historically, it has been shown that patients with testicular cancer with a history of UDT have a greater rate of seminoma than patients with descended testes. However, in these studies, patients with a benign tumor on pathology were excluded from analysis. At this time, there are few contemporary studies that examine the effect of orchidopexy on testicular tumor pathology, inclusive of patients who have a benign testicular tumor. This study aimed to identify if surgically treated cryptorchidism correlated with testicular tumor pathology at presentation, risk category, and overall survival.
METHODS: An institutional database of patients treated for testicular cancer was reviewed from 2003-present. Inclusion criteria included testis tumor patients who had undergone an orchiectomy. Exclusion criteria included unknown cryptorchidism history, unknown pathology, or laterality of orchiectomy. Data collection included demographics, surgical history, tumor marker status, testicular cancer staging, and survival. Patients were placed into risk categories based on International germ cell cancer collaborative group classifications with very low risk patients including those with Stage I-IIB.
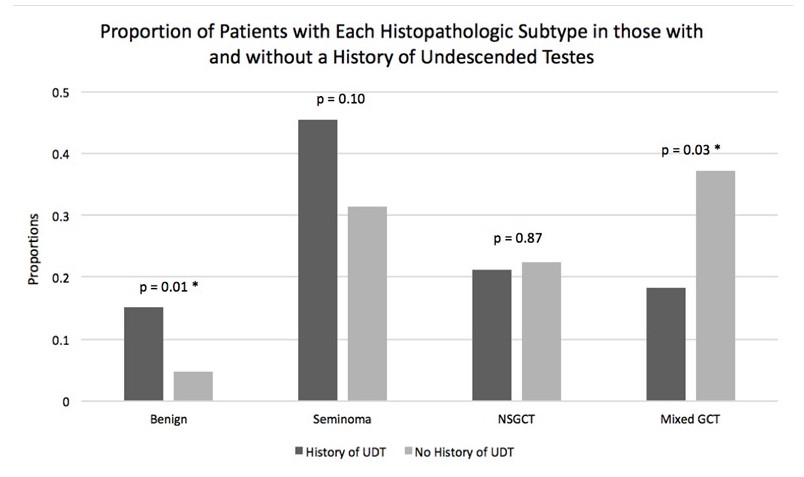
RESULTS: A total of 435 patients were identified that met inclusion criteria, 33 of these patients had a history of UDT. There was no statistical difference in age at orchiectomy, laterality of orchiectomy, or lymphovascular invasion in regards to UDT history. There was a statistical difference in the pathology of testis after orchiectomy, p = 0.03, see table. On further analysis using a 2-sample test of proportions, there was a statistically significant difference in the rate of benign pathology in patients with a history of UDT (15.2%) compared to those without a history of UDT (4.7%), p = 0.01. There was also a statistically significant difference in the proportion of patients with mixed GCT in patients with a history of UDT (18.2%) compared those without a history of UDT (37.3%), p = 0.03. There were no statistically significant differences in other pathology, see figure. There was no difference in risk category or overall survival in patients with or without a history of an UDT.
CONCLUSIONS: Previous studies have shown that there is a greater rate of seminoma in patients with testicular cancer in an undescended testis. This study shows that in patients with a history of UDT compared to those without a history of UDT, there is a greater percentage of patients with benign testicular tumors after orchiectomy. It may be beneficial to consider screening these patients frequently with ultrasound or performing testis sparing surgery rather than proceeding immediately to radical orchiectomy. 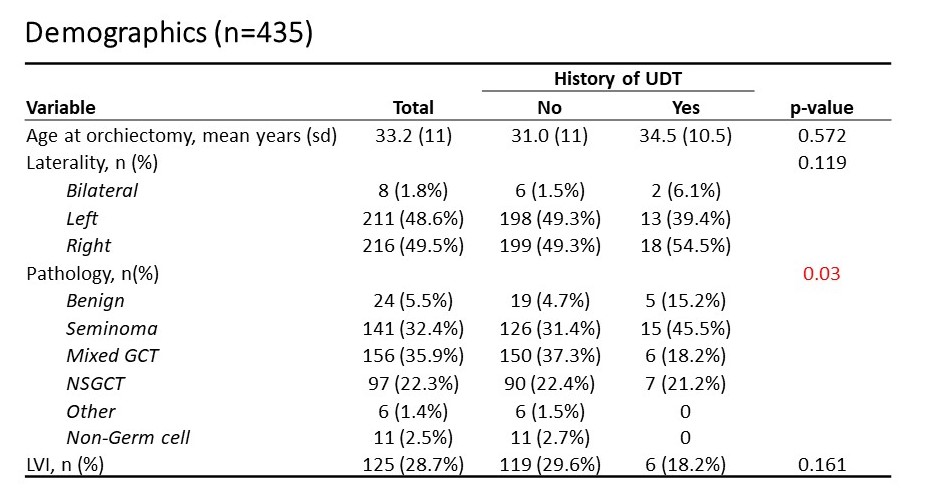
Back to 2019 Abstracts




