What do providers think about shared decision-making regarding hypospadias surgery? Components, applications and barriers to adoption in pediatric urology and general pediatrics
Katherine H. Chan, MD, MPH1, Rosalia Misseri, MD1, Mark P. Cain, MD1, Benjamin Whittam, MD1, Konrad Szymanski, MD, MPH1, Martin Kaefer, MD1, Richard Rink, MD1, Brandon Cockrum, MFA2, Courtney Moore, BA2, Sarah Wiehe, MD, MPH2.
1Department of Urology, Division of Pediatric Urology, Indiana University School of Medicine, Indianapolis, IN, USA, 2Department of Pediatrics, Children's Health Services Research Center, Indiana University School of Medicine, Indianapolis, IN, USA.
Background: Many parents experience decisional conflict (DC) and decisional regret (DR) when making decisions about hypospadias surgery and other reconstructive operations. Although the utilization of a shared decision-making (SDM) process may mitigate these issues, addressing the principal components of the SDM process is a complex task that requires the investment of providers. The purpose of this study was to facilitate a discussion about SDM regarding hypospadias surgery with pediatric urology and general pediatric providers to explore components, clinical applications and barriers to adopting SDM in clinical practice.
Methods: We conducted two workshops with researchers, pediatric urology providers and general pediatric providers, engaging them in guided discussions to explore components, clinical applications and barriers to adopting SDM regarding hypospadias surgery. All activities were audio recorded and professionally transcribed. The transcripts were analyzed using qualitative content analysis to identify key themes and relationships between themes to form the development of an affinity diagram (Figure 1).
Results: We conducted two co-design workshops in November 2018 and January 2019 respectively, one with pediatric urology providers (n=7) and one with general pediatric providers (n=10): median age 47.5 years, 83.3% Caucasian, 58.3% male, 58.3% MD's and 41.7% nurse practitioners. Both groups identified the following components of SDM: a) engaging families and facilitating discussion, b) informing them about treatment options including risks and benefits and c) eliciting values/preferences, concerns and goals of care (Figure 1). Urology providers also suggested that consultation between providers about challenging cases is a type of SDM. Both groups thought that SDM was useful for: a) discussion of preference-sensitive conditions such as hypospadias (i.e. conditions for which there is more than one reasonable management option), b) assessment/encouragement of parental compliance and c) affirmation of a parent's choice to observe (versus treat) a medical condition. General pediatric providers also suggested that SDM was useful for avoiding unnecessary referrals to specialists. Both groups identified the following barriers to the adoption of SDM: a) parental lack of interest and/or desire for paternalism, b) parental misperceptions about medical evidence and c) parent already having made a treatment decision prior to the visit with the provider. The urology providers also noted that time constraints and productivity pressures were significant barriers to SDM adoption in clinical practice.
Conclusions: Providers who care for hypospadias patients are knowledgeable about SDM and its potential clinical applications. They identified several potentially modifiable barriers to the adoption of a SDM process about hypospadias surgery in a pediatric clinical setting. Based on their feedback, we plan to implement a hypospadias decision aid early in the parental decision-making process about hypospadias such as in the postpartum unit and at well-child visits in the newborn period. (Figure 1: red=pediatric urology providers, blue=general pediatric providers, purple=both) 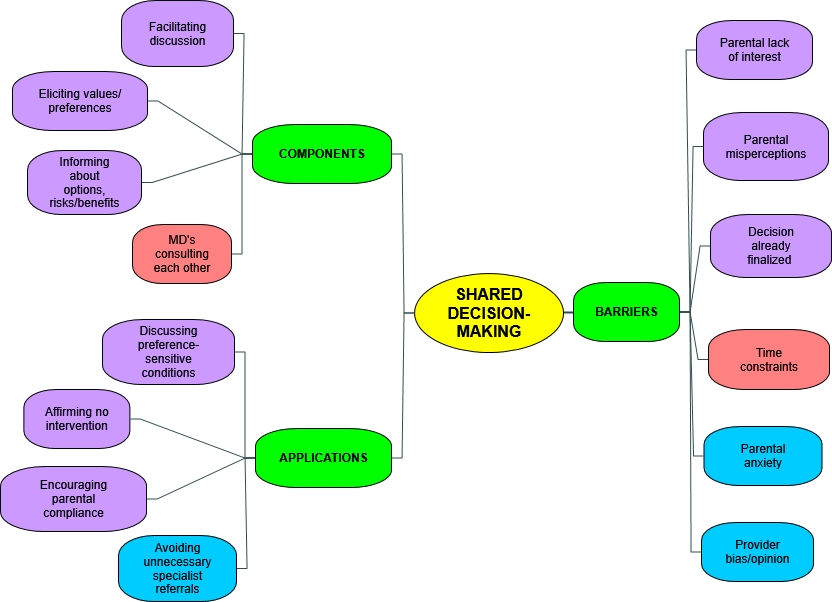
Back to 2019 Abstracts




