Preoperative Bladder Bowel Dysfunction is the Most Important Predictive Factor for Postoperative Urinary Retention after Robot Assisted Laparoscopic Extravesical Ureteral Reimplantation: a Multi-center Study
Sang Hoon Song, MD., Ph.D.1, Il-Hwan A. Kim, Research Assistant1, Jae Hyun Han, MD2, Kun Suk Kim, MD., Ph.D.2, Esther J. Kim, B.S.1, Kunj Shesth, MD1, Jonathan Gerber, MD1, Minki Baek, MD., Ph.D.3, Chester Koh, MD1.
1Division of Pediatric Urology, Department of Surgery, Texas Children's Hospital/Scott Department of Urology at Baylor College of Medicine, Houston, TX, USA, 2Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea, Republic of, 3Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of.
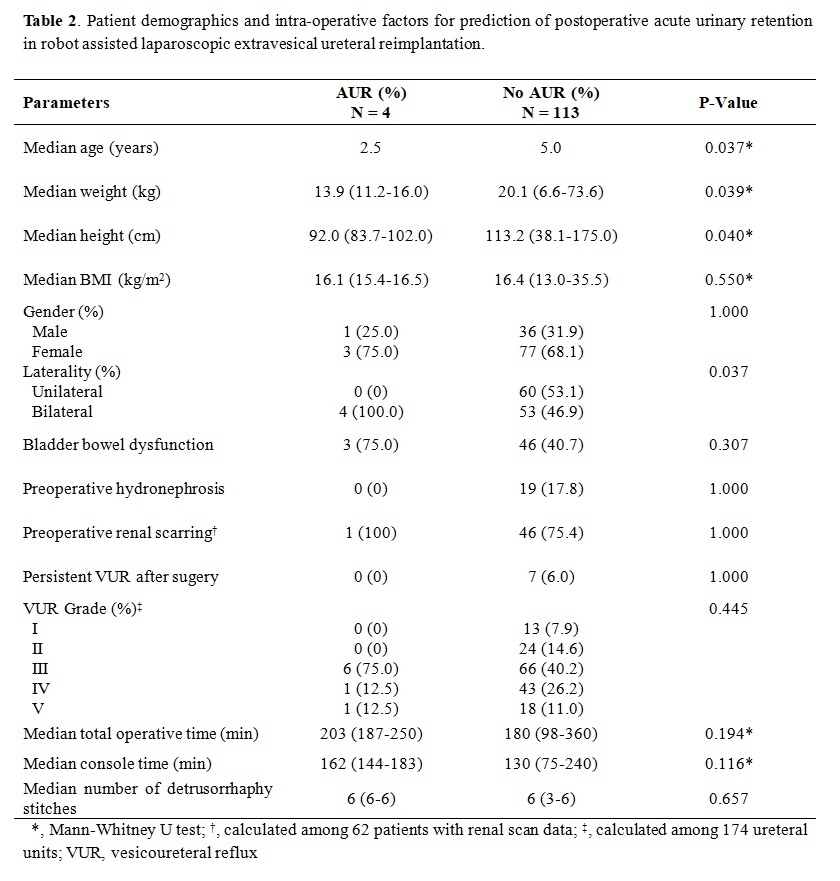
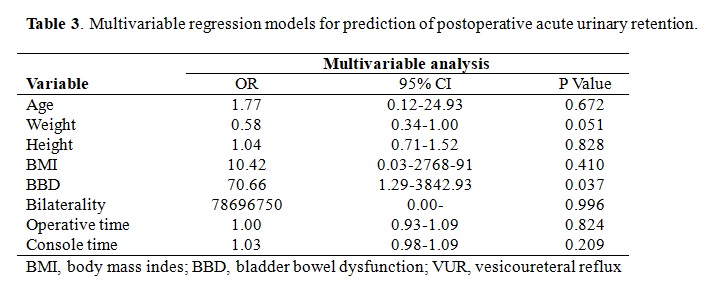
BACKGROUND: Robot-assisted laparoscopic extravesical ureteral reimplantation (RALUR-EV) has been reported as a viable minimally invasive surgical option for vesicoureteral reflux (VUR) with comparable success rates to open reimplantation at several pediatric hospitals, but postoperative acute urinary retention (pAUR) is a known occurrence after both open reimplantation and RALUR-EV. Although bilateral reimplantation was previously described as the most important prognostic factor for pAUR, male gender and length of surgical time but not laterality of reflux were also reported as predictors of pAUR after RALUR-EV in a recent study. We aimed to evaluate the predictive factors for pAUR after RALUR-EV. METHODS: Data for this multi-institutional retrospective cohort study of RALUR-EV patients was obtained from two tertiary referral hospitals. We collected perioperative data including age, gender, body mass index (BMI), bladder bowel dysfunction (BBD) status, VUR grade, laterality of VUR, operation time, the number of detrusorrhaphy stitches, length of hospital stay and postoperative complications. pAUR was defined as the need for urethral catheter replacement after the operation. In patients with pAUR, the urethral catheter was left in place for 2 weeks then subsequently removed with self-voiding afterwards in all cases. Univariate and multivariate analysis was performed to identify predictive factors for postoperative AUR. RESULTS: A total of 117 patients with 174 ureteral units from the two hospitals were enrolled in this study. Patients' demographics between the two hospitals regarding age, weight, height, preop hydronephrosis, BBD rate, VUR grade, console time, and number of detrusorrhaphy stitches are listed in Table 1. Mean age at the time of surgery was 6.1 ± 3.9 years. Bilateral RALUR-EV was performed in 57 (48.7%) cases. pAUR rate was 3.4% in all patients and 7.0% in 57 patients with bilateral VUR (Table 2). All 4 cases of pAUR occurred after bilateral surgery. Univariate analysis showed age (P = 0.037), weight (P = 0.039), height (P = 0.040), and bilaterality (P = 0.037) as predictive factors of pAUR. In a multivariate analysis, weight approached statistical significance (P = 0.051) while BBD was the only significant predictor of pAUR (P = 0.037) (Table 3). CONCLUSIONS: Urinary retention after RALUR-EV less frequently occurred when compared to the previously reported open surgery series. pAUR occurred only in bilateral cases. Preoperative bladder bowel dysfunction but not male gender or surgical time was the most important predictive factor for pAUR after RALUR-EV. 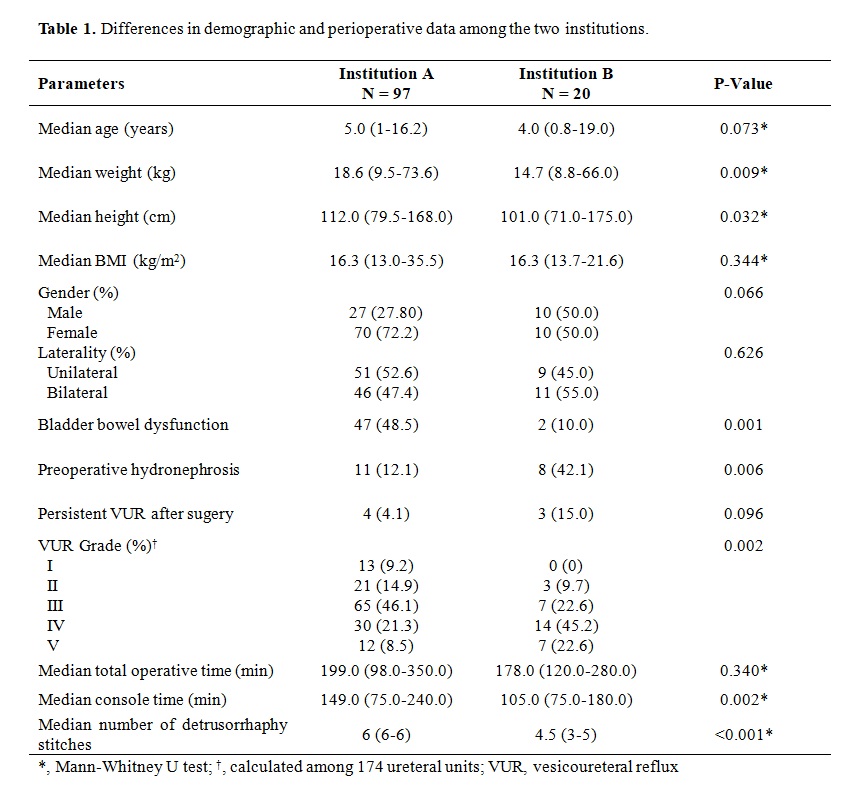
Back to 2019 Abstracts




