Surgical outcomes are equivalent after pure laparoscopic and robotic-assisted pyeloplasty for ureteropelvic junction obstruction
Kristin M. Ebert, MD, Lauren Nicassio, BS, Seth A. Alpert, MD, Christina B. Ching, MD, Daniel G. DaJusta, MD, Molly E. Fuchs, MD, Daryl J. McLeod, MD, Venkata R. Jayanthi, MD.
Nationwide Children's Hospital, Columbus, OH, USA.
Background:
Minimally invasive (robotic and pure laparoscopic) pyeloplasty has been increasingly used for treatment of ureteropelvic junction obstruction (UPJO). However, no large-scale studies have compared these two modalities directly.
Methods:
We performed a retrospective single center review of all patients who underwent pure laparoscopic or robotic pyeloplasty between 2013 and 2018. Only initial pyeloplasty patients were included; patients requiring redo surgery were excluded. Patients were also excluded if they lacked follow-up. Primary outcomes of interest included operative time, length of stay, and complication rates, including rates of secondary procedures. Operative time was defined as time from procedure start to finish, inclusive of all ancillary aspects such as the performance of retrogrades as well as repositioning and docking. We compared these outcomes between the laparoscopic and robotic groups using Student's t test for continuous variables and a Chi-square for categorical variables.
Results:
A total of 313 patients were identified. Seventy-nine were excluded based on study criteria, and therefore our total cohort was 234 patients: 119 robotic cases and 115 laparoscopic cases. Overall mean postoperative follow-up time was 20.8 months (STD 18.1), with no significant differences between groups in length of follow-up.
Clinical data and outcomes are presented in Table 1. Operative time was significantly shorter in the laparoscopic group when compared the robotic group (3.12 hours vs. 3.75 hours, p<0.001). There were no significant differences between groups in length of stay (1.22 days vs 1.50 days, p=0.095). Complications occurred in 65 patients (27.8% of overall cohort); there were no significant differences between groups in overall complication rates. Infectious complications (including both febrile and non-febrile urinary tract infections) occurred in 27 patients (11.5% of total cohort), again with no significant differences between groups. Twenty-four patients (10.3% of total cohort) required at least one secondary procedure. Three patients, all in the laparoscopic group, required nephrostomy tube placement for urine leak; one went on to develop recurrent obstruction. Sixteen patients, 8 in the robotic group and 8 in the laparoscopic group, required at least one secondary procedure for recurrent obstruction. Eight of these (4 in each group) were managed endoscopically alone, and eight (4 in each group) required redo pyeloplasty. Six patients had secondary procedures for other reasons.
Conclusions:
We found no evidence to suggest there are better surgical outcomes with robot-assisted pyeloplasty, suggesting equipoise between both modalities. In a time where emphasis is placed on advancing surgical technology, standard laparoscopic techniques should continue to play an important role in the treatment of UPJO for surgeons trained in this modality, especially in countries where robotic technology may not be readily available. 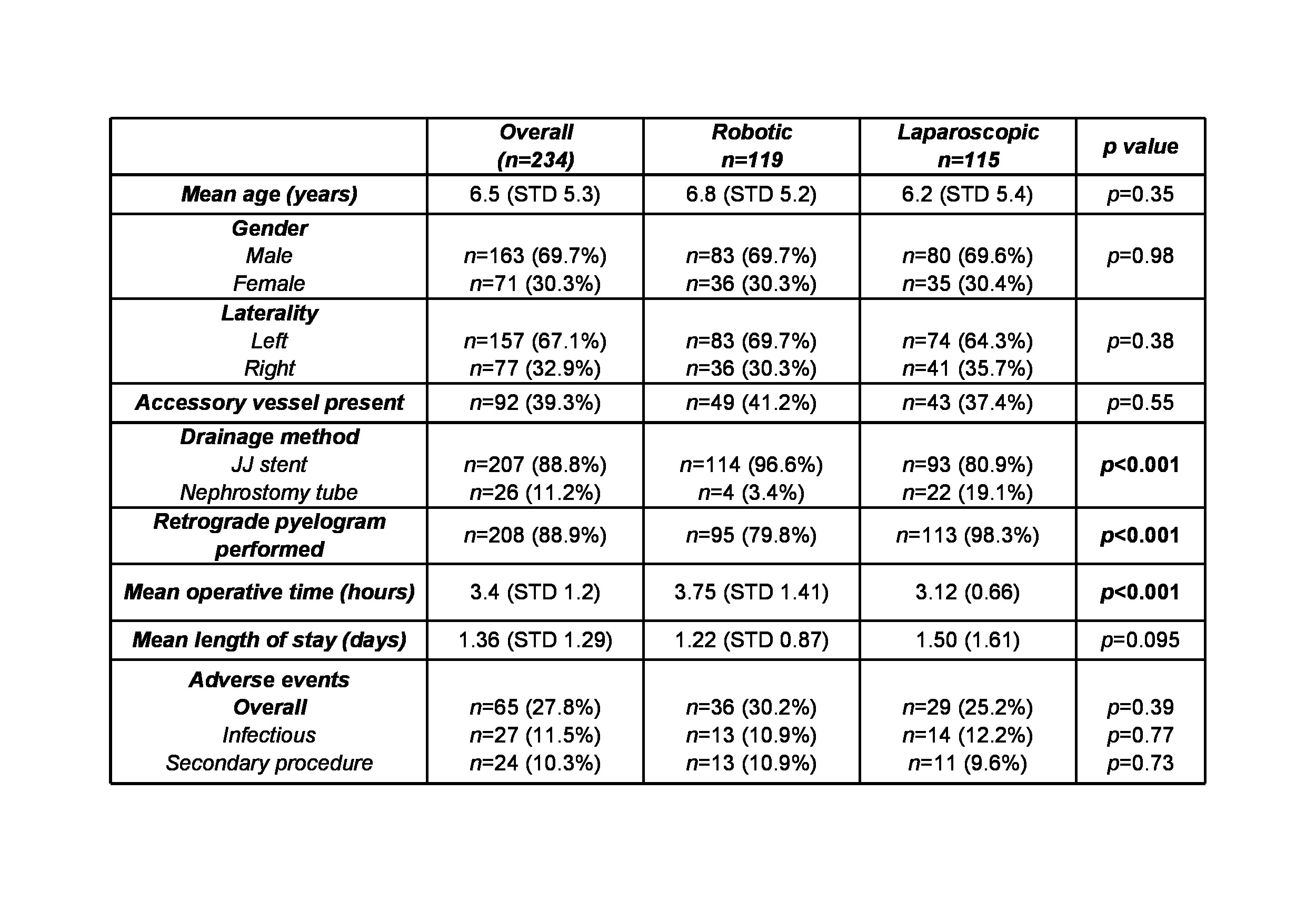
Back to 2019 Abstracts




