Workforce Diversity and Mentorship in Pediatric Urology: Achieving, Retaining, Growing
Ilina Rosoklija, MPH1, Emilie K. Johnson, MD, MPH1, Diana K. Bowen, MD1, Christina B. Ching, MD2, Jonathan S. Ellison, MD3, Nicholas M. Holmes, MD, MBA4, Venkata R. Jayanthi, MD2, Alison C. Keenan, MD5, Elizabeth Malm-Buatsi, MD6, John C. Pope, MD7, Stacy T. Tanaka, MD, MS7, Lily C. Wang, MD, PhD8, Elizabeth B. Yerkes, MD1.
1Ann & Robert H. Lurie Children's Hospital, Chicago, IL, USA, 2Nationwide Children's Hospital, Columbus, OH, USA, 3Children's Hospital of Wisconsin, Milwaukee, WI, USA, 4Rady Children's Hospital, San Diego, CA, USA, 5Atrium Health, Charlotte, NC, USA, 6University of Missouri Department of Surgery-Urology Division, Columbia, MO, USA, 7Vanderbilt University Medical Center, Nashville, TN, USA, 8Valley Children's Hospital, Madera, CA, USA.
Background: The 2019 Societies for Pediatric Urology (SPU) meeting included a panel discussion about maximizing the talents of pediatric urologists from diverse backgrounds. A pre-panel survey was administered to characterize current demographic trends and professional experiences among pediatric urologists who are members of the SPU.
Methods: An IRB-approved, anonymous, online survey was sent to all SPU members. Survey development was an iterative process involving input from the entire panel. Multiple-choice and Likert-type questions on demographics, scope of practice, job satisfaction, experience with bias, and views on mentorship were administered. Descriptive statistics were used to analyze survey data, and subgroup analyses were performed for gender (male vs. female) and years in practice (≤10 vs. >10). Fisher's exact was used for comparative analyses.
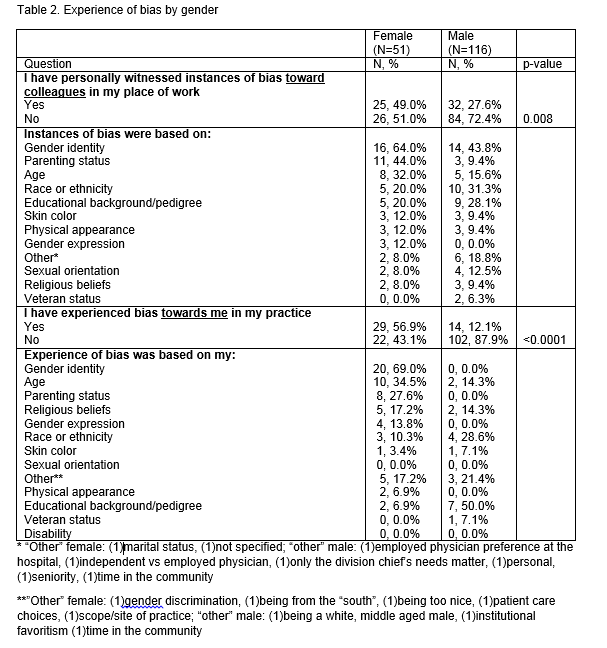
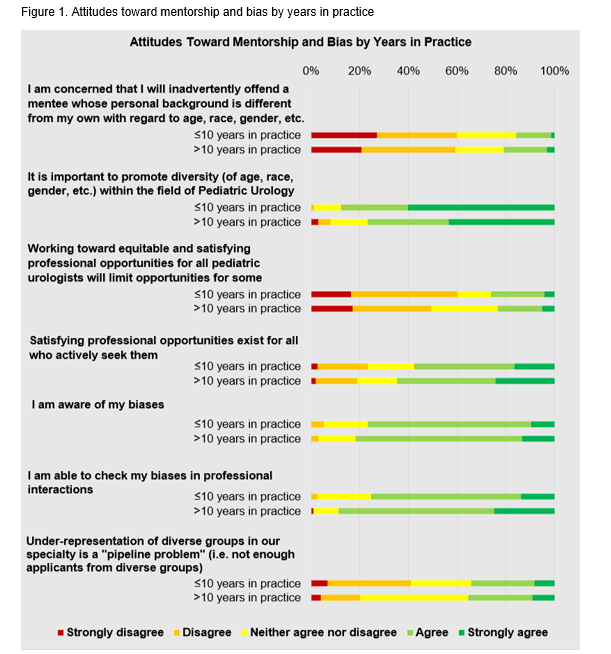
Results: 711 SPU members were contacted, 251 (35%) opened the email and of those 188 (75%) responded to the survey. 67% of respondents were male, 93% heterosexual, 73% white, 8% Hispanic, 88% married and 74% were the primary financial provider in their household. 69% practiced in an academic setting and 61% were in a practice with 1-4 urologists. 26% were in practice <5 years, 17% 5-10 years and 58% >10 years. Females were more likely to be in practice for ≤10 years (p<0.0001). Factors in selecting a first position and practice scope determination are listed in Table 1. No differences were seen between responses when stratified by gender or years in practice. Females were more likely to report witnessing bias toward colleagues and themselves. Both males and females reported witnessing the highest likelihood of bias toward others based on "gender identity." Females were also likely to witness bias toward others and themselves based on "parenting status" and "age," while males were likely to witness bias toward others and themselves based on "race/ethnicity" and "educational background/pedigree" (Table 2). 40% of respondents considered themselves "mentors," 8% "mentees," and 46% "both." 87% felt that mentoring younger pediatric urologists should be an "important part of [their] job". 82% of all respondents agreed that it is important to promote diversity in Pediatric Urology. Attitudes toward mentorship, diversity and bias were similar irrespective of years in practice (Figure 1).
Conclusions: Survey responses reflected increasing diversity in pediatric urology. Respondents represented the spectrum of years in practice, but the number of females in the first 10 years in practice showed a trend in gender diversity. Respondents largely affirmed the professional obligation to mentor younger urologists, but perceived challenges in mentorship were raised by some. Our findings illustrate opportunities for continued progress in the areas of mentorship and bias. 
Back to 2019 Abstracts




