Collaboration and Standardized Management Plans to optimize clinical care and research of Posterior Urethral Valves
Daryl J. McLeod, MD MPH1, Alexandra Rehfuss, MD1, Pramod Reddy, MD2, Candace Granberg, MD3, Brian VanderBrink, MD2, Benjamin Whittam, MD4, Edward Gong, MD5.
1Nationwide Children's Hospital, Columbus, OH, USA, 2Cincinnati Children's Hospital, Cincinnati, OH, USA, 3Mayo Clinic Children's Center, Rochester, MN, USA, 4Riley Children's Hospital, Indianapolis, IN, USA, 5Lurie Children's Hospital, Chicago, IL, USA.
BACKGROUND: Posterior Urethral Valves (PUV) is a rare, yet devastating disease of the urinary tract with the potential for significant kidney injury. An estimated 30-40% of children with PUV will ultimately progress to end stage renal disease (ESRD). Mechanisms for ESRD progression are multifactorial and likely result from a combination of baseline renal dysplasia, persistent obstruction, hostile bladder, and recurrent infections. Unfortunately, significant variability exists across US pediatric centers in the management of PUV, which impedes optimization of care. Standardized Clinical Assessment and Management Plans (SCAMPs) were first described by the cardiovascular department at Boston Children's Hospital in 2010 and have since shown to reduce practice variation, resource utilization and cost of care. SCAMPs improve on clinical practice guidelines by inviting clinician diversions, data collection and outcome measures. Through a multispecialty and multi-institutional collaborative we aimed to 1) assess the need for and 2) develop a SCAMP for the management of PUV across five Midwest children's hospitals.
METHODS: Pediatric Urology Midwest Alliance (PUMA), a multispecialty and multi-institutional clinical and research collaborative was initiated in 2017 with the goal of improving the management and investigation of rare urologic diseases. PUMA identified PUV as an optimal disease process for investigation under this mission with the goal of an initial retrospective analysis of our combined patient cohort followed by the development of a PUV specific SCAMP.
RESULTS: A retrospective analysis identified 274 children born between 1995 and 2005 with PUV who were initially cared for at one of the five PUMA centers. On survival analysis, 30% progressed to ESRD by 15 years of age. Further investigation of this cohort identified significant practice variability between PUMA centers for utilization and timing of urodynamic testing, clean intermittent catheterization, renal scintigraphy, voiding cystourethrogram and anticholinergic and alpha-blockade medications. Next, through surveys, we collated the general practice of pediatric urologists at the individual PUMA centers to determine a "heat map" of our individual practices (Figure). In areas of disagreement, literature review, conference calls and in-person meetings facilitated consensus. In order to optimize acceptance, surgeon preference options were included where a practice outlier was encountered. Analysis of surgeon preference options and variance off SCAMP will occur after every 100 patients. The SCAMP will then be revised in accordance with best patient outcomes.
CONCLUSIONS: To date we have shown the feasibility for multispecialty and multi-institutional collaboration for the management of a rare disease. This SCAMP represents, to our knowledge, the most comprehensive, evidence based management pathway available for the care of PUV. Future work is ongoing to implement this newly developed SCAMP across all five PUMA centers and to record surgeon preference options, SCAMP diversions and outcomes, with the ultimate aim of decreasing progression to ESRD in PUV. 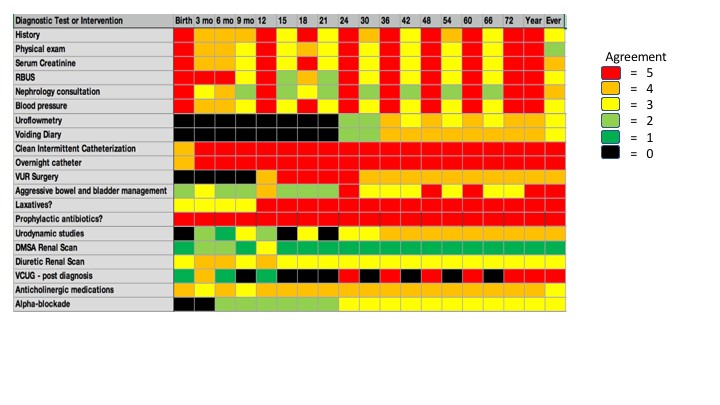
Back to 2019 Abstracts




