Post-procedural complication rates and utilization of health care between gomco and plastibell office circumcision techniques
Lauren Nicassio, BS, Yuri V. Sebastiao, PhD MPH, Molly Fuchs, MD, Daryl McLeod, MD MPH, Seth Alpert, MD, Rama Jayanthi, MD, Christina B. Ching, MD, Daniel DaJusta, MD.
Nationwide Children's Hospital, Columbus, OH, USA.
BACKGROUND: Gomco clamp and plastibell ring are common methods of performing office circumcision. While there are similar features between the two, they do differ significantly, in that the plastibell is retained upon office discharge versus immediate office removal of the gomco device. We sought to evaluate the rate of early complications and impact on health care utilization of these two forms of office circumcision.
METHODS: We performed a retrospective review of all office circumcisions performed in our urologic clinic between January 2015 - August 2018. Patient demographics, circumcision technique, provider information, and any subsequent telephone encounters or hospital visits were recorded. Complications related directly to circumcision were noted and reported as early complications if they occurred within 14 days of circumcision. Number of phone calls, emergency room (ER) and urgent care (UC) visits, trips to the operating room (OR), and office visits outside of those scheduled as per post-circumcision routine that were directly related to their circumcision were recorded. Frequencies were used to compare the incidence of early postoperative complications, emergency visits, and interventions, by circumcision technique using propensity score-inverse probability of treatment weights. This approach allowed estimating the adjusted effect of circumcision technique while controlling for baseline differences in patient age, weight, comorbidities, and provider characteristics.
RESULTS: A total of 1030 circumcisions were performed in the study period. Overall median patient age and weight were 10 weeks (range 0.6-56.9) and 5.7 kg (range 3.0-13.1), respectively. Approximately 65% (665 cases) of the procedures were performed by plastibell, with 35% (365 cases) by gomco. There was no significant difference between plastibell and gomco techniques in regards to early complications (3.1% vs. 2.5% respectively, p=0.61); need for office, ER, or OR interventions within 14 days (4.4% vs. 4.1%, p=0.83); or number of patients visiting the ER/UC within 14 days of circumcision (3.6% vs. 1.7%, p=0.10) (Table). In total, 18 patients (2.7%) had a plastibell malfunction with 17 requiring provider removal of the ring. There were 139 (20.9%) office phone calls by parents of patients after plastibell circumcision versus 65 (17.8%) from parents after gomco. 35 (9.6%) gomco patients required a non-routine postoperative office visit versus 32 (4.8%) plastibell patients.
CONCLUSIONS: In this single-institution cohort of children undergoing office circumcision, the use of gomco versus plastibell technique was not associated with significant differences in early postoperative complications. Plastibell appears to result in more phone calls while gomco results in more office visits outside of that which is normally planned after the procedure. This knowledge could lend to better education at time of office circumcision regarding expectations. 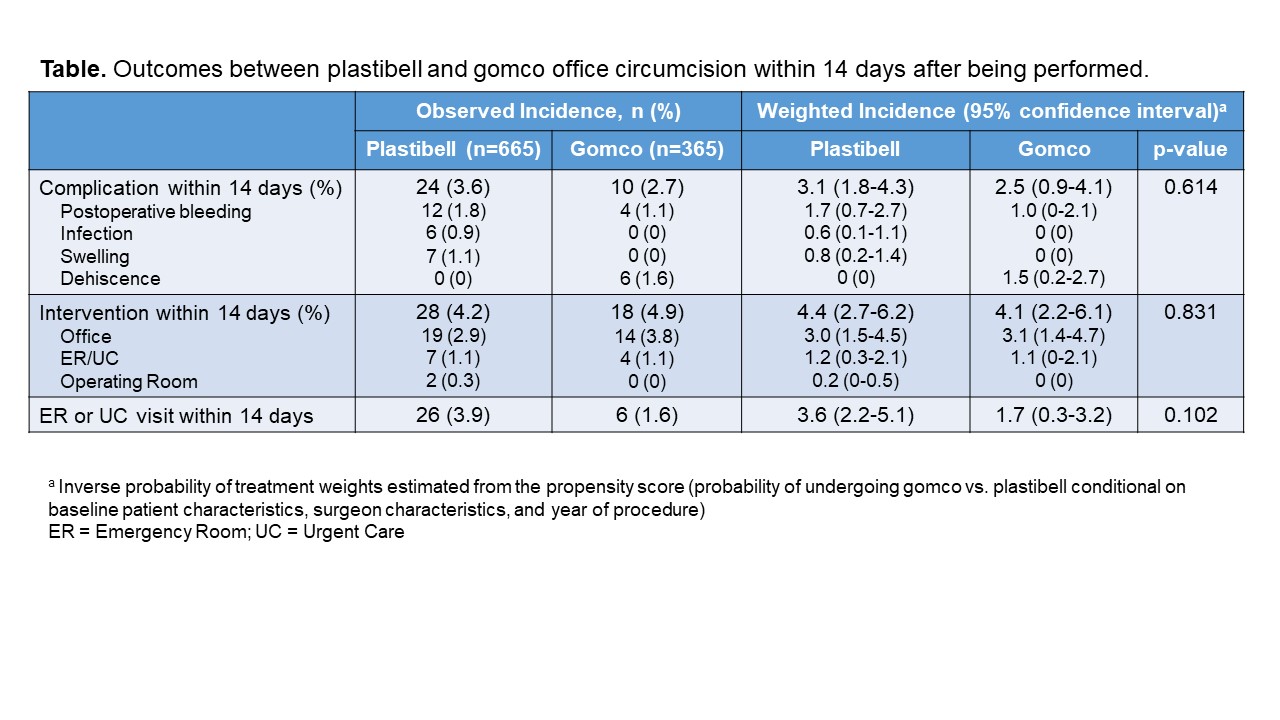
Back to 2019 Abstracts




