Inability to adequately buffer trans IL-6 signaling may play a role in development of renal scarring after urinary tract infection
Guillermo Yepes Junquera, MD, Sudipti Gupta, PhD, Lauren Nicassio, BS, Brian Becknell, MD PhD, Christina B. Ching, MD.
Nationwide Children's Hospital, Columbus, OH, USA.
Background: While inflammation is an important innate defense mechanism in the setting of infection, it can also lead to local tissue damage. Interleukin (IL)-6 is a known mediator of inflammation, particularly through its trans signaling pathway. We hypothesized that activation of the trans IL-6 signaling pathway would be associated with the development of renal scarring. We evaluated markers of trans IL-6 signaling between patients with a history of UTI with and without renal scarring.
Methods: As part of an IRB-approved protocol, we collected urine samples in assenting/consenting pediatric patients with a history of culture positive UTI (>50K uropathogen on culture) being evaluated in the urology clinic with documented presence or absence of renal scarring on imaging (renal ultrasound and/or DMSA). A group of healthy control (HC) urines in patients without a history of UTI and without concern for current UTI being seen in the urology clinic were also collected. Enzyme-linked immunosorbent assays were performed on samples looking at markers of trans IL-6 signaling such as IL-6 and IL-6 receptor (R), including sgp130 which is a buffer in trans IL-6 signaling. These values were normalized to urine creatinine. Results were analyzed by t-test or Mann-Whitney U using Graphpad software. A p-value of <0.05 was considered significant.
Results: A total of 69 urines from patients with a history of UTI were collected: 25 with and 44 without scarring. The median age of those scarred versus not scarred was 7.9 vs 6.4 years (p=0.3469); 22 (88%) of those scarred and 41 (93%) of those not scarred were female (p=0.6603). 13 urine samples from HC were collected. All of these patients were male. These patients were significantly younger than those with a history of UTI (median age 3.5 years, p=0.0077). While there was no significant difference in IL-6, IL-6R, or sgp130 between those with a history of UTI who were scarred versus those not scarred, there was significantly more IL-6 in the urine of those with a history of UTI regardless of presence of scarring versus HC and significantly less sgp130 in those scarred compared to HC (p=0.0157) (Figure). While there was less sgp130 in the scarred versus not scarred patients with a history of UTI, it did not reach significance (10,905 pg/mg versus 13,885 pg/mg, p=0.1446).
Conclusions: Trans signaling may play a role in the development of renal scarring based on those who develop renal scarring having less sgp130, a buffer for the trans signaling pathway. Manipulation of the buffering system to control trans IL-6 signaling may be a method to reduce the sequela of renal scarring in UTI. 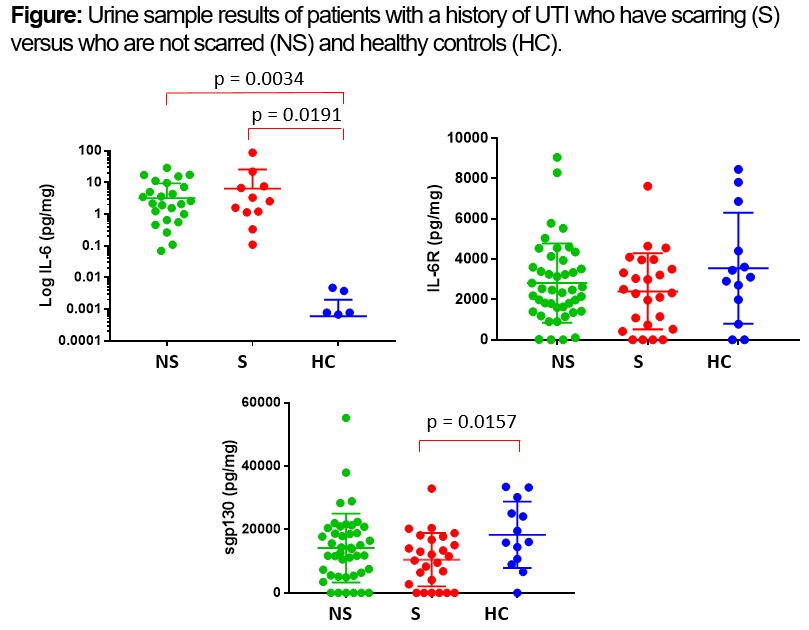
Back to 2019 Abstracts




