Outcomes of Deflux Treatment for Vesicoureteral Reflux Follwing Pediatric Renal Transplant: A Systematic Review
Karla Rebullar, MD1, Fardod O'Kelly, MD1, Armando J. Lorenzo, MD, MSc, FRCSC, FAAP, FACS1, Rusul Al-Kutbi, MD1, Andrew J. Kirsch, MD, FAAP, FACS2, Martin A. Koyle, MD, MSc, FAAP, FACS, FRCS (Eng.), FRCSC1, Fadi Zu'bi, MD1.
1Division of Urology, The Hospital For Sick Children, Toronto, ON, Canada, 2Department of Pediatric Urology, Children's Healthcare of Atlanta,, Atlanta, GA, USA.
Introduction
Vesicoureteral reflux (VUR) after renal transplant in the pediatric population, may be associated with an increased incidence of symptomatic urinary tract infection (UTIs) leading to increased morbidity, hospitalizations and costs.
The "non-orthotopic" location of the transplanted donor ureter and the abnormal bladder support of the tunnel may pose challenges in correcting the VUR using minimally invasive endoscopic injection techniques. Herein we report the results of a systematic review evaluating the outcomes of endoscopic treatment of VUR using Deflux as the bulking agent, in post-renal transplant pediatric patients.
Methods
Pubmed/Medline and Embase databases were searched from the FDA approval date of Deflux in 2001 until April 2019. Only full-text English articles involving patients less than 18 years old at the time of transplant, with a diagnosis of VUR post-transplantation, who underwent Deflux treatment were included. Figure 1 outlines our search strategy. Quantitative analysis was done using SPSS 23.0.
Results
We found only 6 eligible studies describing Deflux treatment outcomes in 67 pediatric patients with post-transplant VUR (2008-2019) where voiding cystourethrogram (VCUG) confirmed the diagnosis and reported the resolution of VUR in all cases.
Mean success rate, defined as VUR resolution at the time of follow up was 36.8% (0%-63.6%), which is lower than the reported 80-85%% success rate with open ureteroneocystotomy (UNC). Ureteral obstruction occurred in 7/67 cases (11.3%), fat higher than that reported for injection techniques for VUR in non transplant situations. Endoscopic ureteric stenting was the initial management in all presumed cases of obstruction, but was only successful in 1 patient (14%). Open ureteral reimplantation was performed in 4 cases (57%), while 2 were managed expectantly (29%, unknown outcomes).
Persistent VUR with UTI despite Deflux were reported in 20 cases. Of these, 7 (35%) were managed with instituting prophylactic antibiotics, and 13 (65%) with open ureteroneocystostomy (UNC). Success rates were consistently low for UNC after failed Deflux (40 to 50%) in comparison to redo reimplantation in transplant ureters without prior injection (70 to 80%).
Conclusion
We believe that the low success rates following injection techniques for symptomatic VUR after pediatric renal transplant is due to combination of altered ureteral tunnel anatomy, altered bladder pathophysiology and recipient immunosuppression. Although an appealing, non-invasive option, endoscopic correction with Deflux for VUR in transplant ureters may prove counter-intuitive due to the unexpectedly high incidence of obstruction and subsequent less than optimal results if UNC is required. A multi-institutional prospective study with a larger population size (study power) may further elucidate these results. 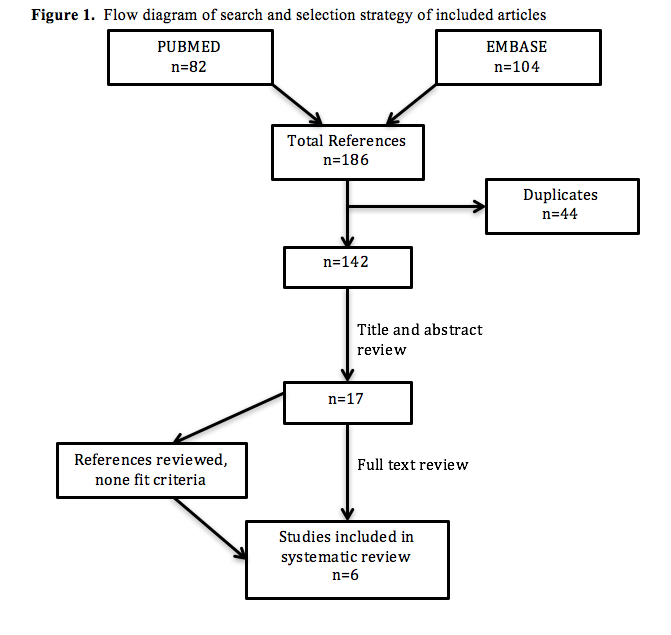
Back to 2019 Abstracts




