Patterns of Lymph Node Sampling and Impact on Survival in Adolescents and Young Adults with Renal Cell Carcinoma: A Surveillance, Epidemiology, and End Result (SEER) Review
Jared Johnson, BA, Jonathan Walker, MD, Megan Eguchi, MPH, Miles Cockburn, PhD, Nicholas Cost, MD.
University of Colorado, Aurora, CO, USA.
BACKGROUND: The incidence of Renal Cell Carcinoma (RCC) in adolescents and young adults (AYA) is reported to be between 0.5-5%. AYA RCC tends to present with higher stage and is more likely to have lymph node (LN) involvement than adult RCC. While nephrectomy with LN sampling is the standard of care, there remains controversy surrounding the extent of LN dissection needed. Recent Children's Oncology Group data demonstrate that complete resection, including all LNs, results in better overall survival (OS). The objective of this study was to describe factors that affect LN sampling, and to determine how LN status and patient/disease characteristics affect OS.
METHODS: The Surveillance, Epidemiology, and End Result (SEER) database was retrospectively analyzed for patients 0-30 years-old with RCC diagnosed between 2004 and 2015. Data was collected on age, gender, race, laterality, stage, histologic type, LNs examined, LNs positive, and surgical approach (nephron sparing (NSS) vs radical nephrectomy). Poisson regression was performed to determine factors associated with number of LNs sampled. Multivariable logistic regression was used to assess patient characteristics on OS. Kaplan-Meier curves were used to present survival trends.
RESULTS: 1268 patients were identified for analysis, with a median age of 27-years (IQR 24-29). Of these, only 237 (18.7%) had LN sampling, and 87 were LN-positive. The most common histology was clear cell (50.5%), followed by RCC NOS (22.6%), chromophobe (12.1%), and papillary (9.9%). Factors associated with fewer LNs sampled included increasing age, right-sided tumors, male sex, smaller tumors, lower stage, NSS (p<0.001), and Hispanic race (p=0.002). Factors associated with decreased 5-year OS included Black race (p=0.039), tumor size (p=0.001), stage III and IV disease, medullary histology (p<0.001), and complete resection (p=0.046). Five-year OS was found to be 87.98% for all patients and 31.12% for those with LN positivity (figure 1, p<0.001). For patients with positive LNs, the median number of nodes examined was 5 (IQR 1-12.5), and the median number of positive nodes was 2 (IQR 1-7). In this cohort, tumor size, stage IV disease, and medullary (p<0.001) and sarcomatoid (=0.016) histologies were predictive of OS. Number of LNs examined, number of LNs positive, and LN density were not associated with OS in LN-positive patients.
CONCLUSIONS: LN positivity, race, tumor size, stage, and histologic type were significantly associated with decreased 5-year OS; however, total number of LNs examined or LNs positive was not predictive of OS. The majority of patients had no LNs sampled at the time of surgery. Factors associated with LN sampling included age, race, sex, laterality, tumor size, stage, and type of resection. This study supports the need for surgeon education on LN sampling for proper staging and counselling for AYA patients with RCC. 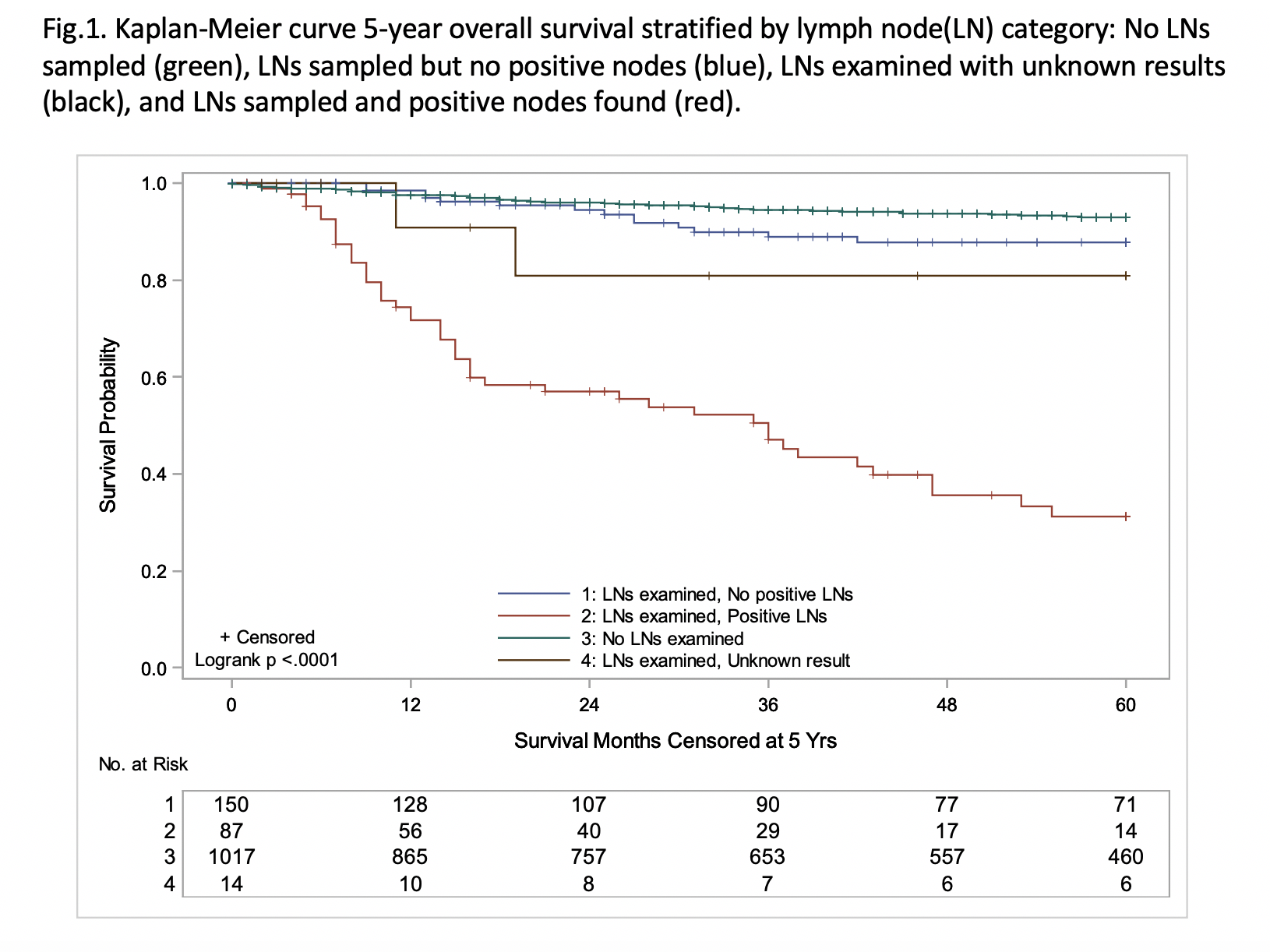
Back to 2019 Abstracts




