Effect of split appendix technique on outcomes of Mitrofanoff channels created at time of genitourinary continent reconstruction
Michael Daugherty, MD, Andrew Strine, MD, Brian VanderBrink, MD, Paul Noh, MD, William R. DeFoor, MD, Eugene Minevich, MD, Curtis Sheldon, MD, Jason Frischer, MD, Pramod Reddy, MD.
Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA.
Background: When creating a catheterizable channel the choice of bowel segment used as a conduit has to be tempered with the morbidity associated with it. The split-appendix technique allows the creation of both a urinary and fecal channel without the need for a bowel anastomosis. However, there is concern that by splitting the appendix there is tenuous blood supply to both channels at completion and may affect outcomes. We aim to compare what affect the bowel segment used for urinary channel at time of reconstruction has on perioperative and long-term outcomes.
Methods: A single institution retrospective review was performed analyzing all patients that underwent simultaneous continent catheterizable urinary channel and a fecal channel at time of reconstruction from the years 2010-2016. Patient demographics, channel characteristics, perioperative complications and clinical success rate were analyzed. Channels were stratified according to how they were created: appendix, split-appendix, Monti. Comparisons between groups were performed using Fisher's exact test for categorical variables and Kruskal-Wallis Test for continuous variables. A multivariate linear regression was performed to identify factors associated with hospital length of stay.
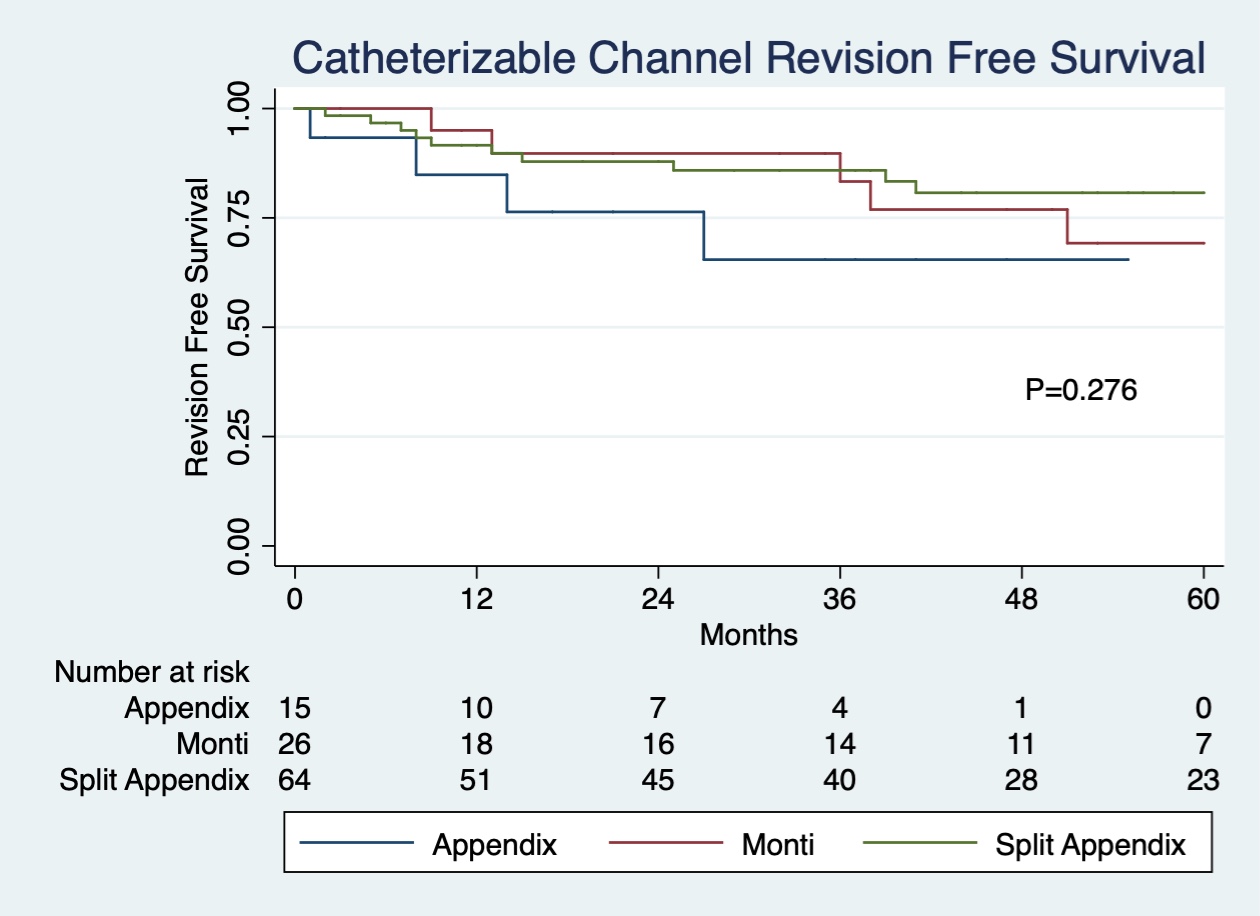
Results: A total of 106 patients were identified in this time period that underwent concomitant urinary and fecal channel at time of reconstruction. The majority of patients (60.4%) underwent a split-appendix technique for channel creation. Those patients undergoing a split-appendix technique had shorter operative times (p<0.00001) with less blood loss (p=0.0001). They also had a shorter hospital stay (p=0.02), while having no change in 30-day complications (Table 1). Median follow-up was 52.5 months, 35 months, and 38 months for the split-appendix, appendix and Monti channels, respectively (p=0.06). There was no difference seen in revision free survival of the channel following surgery (Figure 1). However, there were more subfascial revisions in those undergoing a Monti channel (p=0.001). On multivariable analysis channel type was no longer associated with length of stay, whereas bowel anastomosis at time of surgery and patient age were significant predictors for length of stay.
Conclusions: Utilizing a split-appendix approach for creation of the catheterizable channels does not affect 30-day complications or long-term revision rates. This technique may allow for optimal outcomes while minimizing the morbidity of a bowel anastomosis when technically feasible at time of reconstruction.
| Split Appendix (n=64) | Appendix (n=15) | Monti (n=27) | P-value | |
| Age | 8.7 | 7.6 | 10.7 | 0.015 |
| Gender | 0.007 | |||
| Male | 38 (59.4%) | 5 (33.3%) | 7 (25.9%) | |
| Female | 26 (40.6%) | 10 (66.7%) | 20 (74.1%) | |
| Diagnosis | 0.102 | |||
| ARM | 20 (31.3%) | 9 (60.0%) | 13 (48.2%) | |
| MMC | 34 (53.1%) | 6 (40.0%) | 9 (33.3%) | |
| Other | 10 (15.6%) | 0 (0.0%) | 5 (18.5%) | |
| Ambulatory | 47 (73.4%) | 12 (80.0%) | 21 (77.8%) | 0.824 |
| Weight Status | 0.502 | |||
| Underweight | 2 (3.1%) | 2 (13.3%) | 0 (0.0%) | |
| Normal | 42 (65.6%) | 10 (66.7%) | 20 (74.1%) | |
| Overweight | 10 (15.6%) | 1 (6.7%) | 2 (7.4%) | |
| Obese | 10 (15.6%) | 2 (13.3%) | 5 (18.5%) | |
| Pre-Op CKD | 8 (12.5%) | 1 (6.7%) | 7 (25.9%) | 0.209 |
| Reoperative | 31 (48.4%) | 9 (60.0%) | 15 (55.6%) | 0.70 |
| Bladder Neck Procedure | 37 (57.8%) | 7 (46.7%) | 14 (51.9%) | 0.698 |
| Ureteral Reimplantation | 19 (29.7%) | 6 (40.0%) | 12 (44.4%) | 0.363 |
| Augmentation Cystoplasty | 19 (29.7%) | 5 (33.3%) | 10 (37.0%) | 0.798 |
| Bowel Anastomosis | 23 (35.9%) | 5 (33.3%) | 26 (96.3%) | <0.0001 |
| Median EBL (IQR) | 50 mL (20-100) | 50 mL (25-150) | 150 mL (75-250) | 0.002 |
| Median Operative Time (IQR) | 447 minutes (324-579) | 485 minutes (394-623) | 619 minutes (549-847) | 0.0001 |
| Median Length of Stay (IQR) | 9 days (8-11.5) | 12 days (11-13) | 13 days (11-14) | 0.0001 |
| 30-Day Readmission | 9 (14.1%) | 3 (20.0%) | 4 (14.8%) | 0.799 |
| 30-Day Complications | 22 (34.4%) | 8 (53.3%) | 12 (44.4%) | 0.351 |
| Wound Complications | 8 (12.5%) | 3 (20.0%) | 3 (11.1%) | 0.711 |
| Infectious Complications | 13 (20.3%) | 4 (26.7%) | 9 (33.3%) | 0.400 |
| High Grade Complications | 6 (9.4%) | 3 (20.0%) | 4 (14.8%) | 0.396 |
| Median Follow Up (IQR) | 52.5 months (30.5-79) | 35 months (2-47) | 38 months (3-76) | 0.06 |
| Any Revision | 27 (42.2%) | 5 (33.3%) | 11 (40.7%) | 0.85 |
| Endoscopic Revision | 20 (31.3%) | 3 (20.0%) | 9 (33.3%) | 0.752 |
| Suprafascial Revision | 13 (20.3%) | 4 (26.7%) | 5 (18.5%) | 0.837 |
| Subfascial Revision | 0 (0.0%) | 0 (0.0%) | 5 (18.5%) | 0.001 |
| Multiple Endoscopic Revisions | 8 (40.0%) | 1 (33.3%) | 5 (55.6%) | 0.865 |
| Multiple Suprafascial Revisions | 3 (23.1%) | 0 (0.0%) | 1 (20.0%) | 0.787 |
Back to 2019 Abstracts




