C-tube vs appendicostomy: which one is better for Antegrade Continence Enemas (ACEs)?
Consuelo Sierralta Born, MD, Mandy Rickard, MN, NP, Karen Milford, MD, Joao Amaral, MD, Martin A. Koyle, MD, Armando J. Lorenzo, MD, MSc.
SickKids, Toronto, ON, Canada.
Introduction:
Antegrade enemas have been demonstrated to be efficacious in providing fecal continence in children with a variety of underlying conditions. Two commonly performed procedures to create conduits for antegrade enemas include a catheterizable appendicostomy and placement of a cecostomy tube. Herein, we present our experience with appendicostomy and compare outcomes to those managed with cecostomy tubes.
Methods:
We reviewed the charts of patients undergoing appendicostomy creation or cecostomy tube insertion at our institution between January 2008 and December 2017. We included all patients 0-18 years of age undergoing either procedure by urology, general surgery or image guided therapy (IGT) for any indication. We collected data on age, weight, underlying pathology, surgical variables, length of stay, complications, need for indwelling catheter, need for further procedures and radiation exposure.
Results:
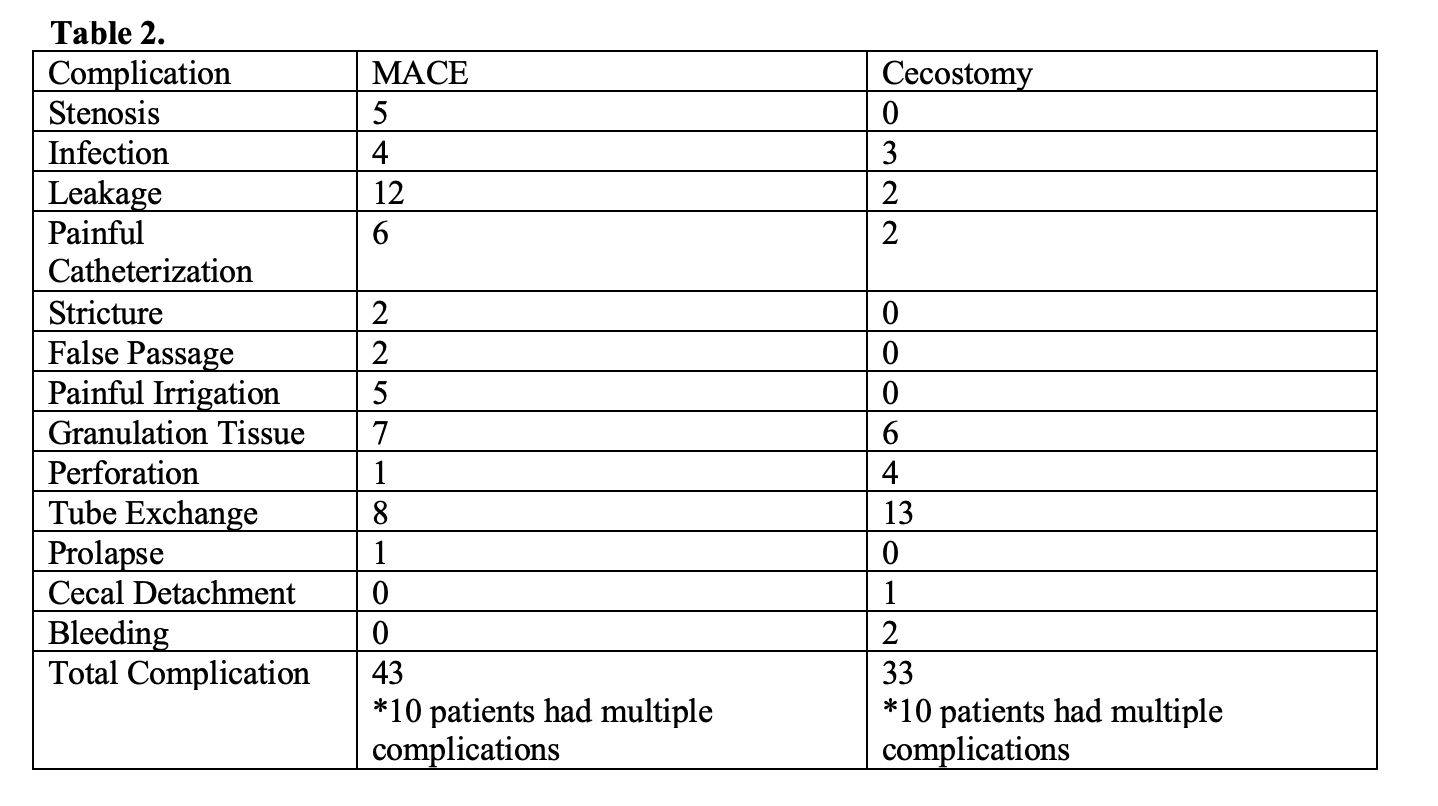
A total of 115 patients were included (63 appendicostomy/52 cecostomy). Sixty-four percent were male, age was 9+4 years and follow-up time was 43+30 months. For appendicostomy patients, the most common indication was neurogenic bowel. Eighty-four percent of these procedures were performed by a urologist and stomal location was most often in the umbilicus (69%). Constipation was successfully managed in 93% of patients and 95% reported compliance with flushes at last follow up. The most common additional procedure was stomal revision (16%, n=10). In 17 cases (27%) an indwelling catheter was placed through the appendicostomy due to inability or difficulty performing intermittent catheterization. For cecostomy tube patients, the primary indication was fecal incontinence (43%). Ninety-six percent of procedures were completed by interventional radiologists and tube placement was in the right lower quadrant (RLQ) in 92% of cases. Cecostomy tube position needed further assessment by radiograph 2+1 times in 58% of patients. Unplanned tube exchanges were necessary in 44%. Constipation was successfully managed in 92% of patients and 89% reported compliance with flushes. The most common additional procedure was cecostomy closure(n=8) and conversion to appendicostomy (n=5). There were no significant differences between groups for most characteristics including the rate of complications (p=0.97). There was a significant difference in length of hospital stay (2.8+3 days vs. 5+5 days) and duration of IV antibiotics (1+1 vs. 5+13 days) in favor of appendicostomy vs. cecostomy respectively. Patient characteristics can be found in Table 1. Complications can be reviewed in Table 2.
Conclusion:
Both appendicostomy and cecostomy procedures are effective at delivery of antegrade enemas for the purposes of bowel management. Whilst complication rates were similar, tube placement and planned and unplanned tube changes result in increased radiation exposure in patients with cecostomies. Additionally, patients undergoing appendicostomy experienced shorter durations of antibiotic use and shorter hospital stays. These data suggest that appendicostomy creation has advantages over cecostomy tube placement, and thus may be favored as first-line intervention. 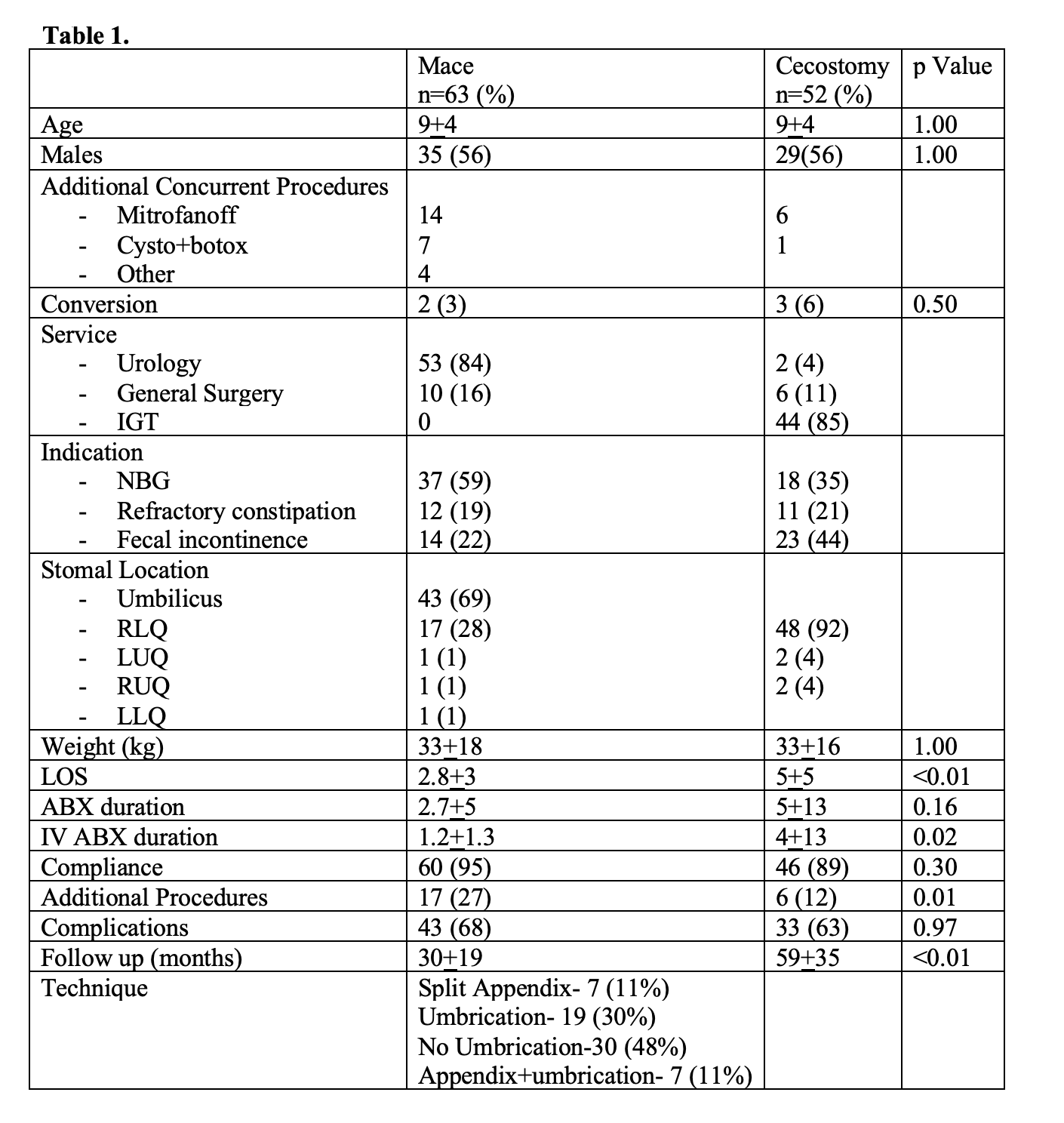
Back to 2019 Abstracts




