Pressure Injury Prevention for Urology Surgical Procedures
Azadeh Wickham, MSN, FNP-BC, Pat Clay, MSN, RN, CWCN, Joel Koenig, MD, Paul Bowlin, MD, Alonso Carrasco, MD, John Gatti, MD.
Children's Mercy Kansas City, Kansas City, MO, USA.
Background:
Pressure Injuries (PI) are one of the leading causes of harm in healthcare settings. However, there are gaps in knowledge in relation to PI prevention in surgical patients, particularly in pediatric surgical patients. In the operating room, several factors such as positioning, anesthesia, duration of surgery, and patient co-morbidities can affect PI development. Perioperative pressure injury is defined in the literature as any pressure related injury, including non-blanchable erythema, purple discoloration, or blistering associated with operating room positioning up to 72 hours postoperatively.
Objectives:
In 2017, a high incidence of perioperative pressure injuries involving cases of urologic reconstruction was noted. January 2018, the Urology department initiated a pressure injury prevention protocol for reconstructive procedures. The goal was to improve identification of at risk patients, perform appropriate interventions related to surgical positioning, and increase staff knowledge and awareness of assessment and prevent preoperative pressure injuries.
Methods:
Patients planning urologic reconstructive surgery are identified and the protocol initiated as follows. A Wound Ostomy and Continence (WOC) consult is initiated during the pre-operative clinic visit or in same day surgery. Guided by the NPUAP (National Pressure Ulcer Advisory Panel) clinical practice guidelines for the operating room, a WOC team member completes a review and assessment of the patient and photographs areas of concern. On the day of surgery, WOC team is paged by same day surgery or the operating room team. The perioperative head-to-toe skin assessment is completed by an operative nurse. A WOC team member positions the patient in the operating suite with the following considerations: time of surgery, potential for friction shear, support surface, and procedure. Following the surgical procedure, the operating room nurse completes a post-operative skin assessment and the patient is transported to the PACU where areas of concern are verbalized and a second skin assessment is completed by a PACU nurse. WOC assesses each patient on post-operative day 1 and the next assessment is completed at the 3 week post-operative clinic visit.
Results:
Prior to initiation of the protocol, as many as 5 pressure injuries were noted per quarter. After initiation of the protocol, we have not experienced a single pressure sore.
Conclusions
Pressure injuries are preventable with employment of a collaborative protocol for pressure injury prevention. Factors of increased awareness, shared ownership and knowledge of pressure injury prevention within the team are likely responsible. This strategy may be useful to other surgical specialties with procedures at high risk for pressure injury. 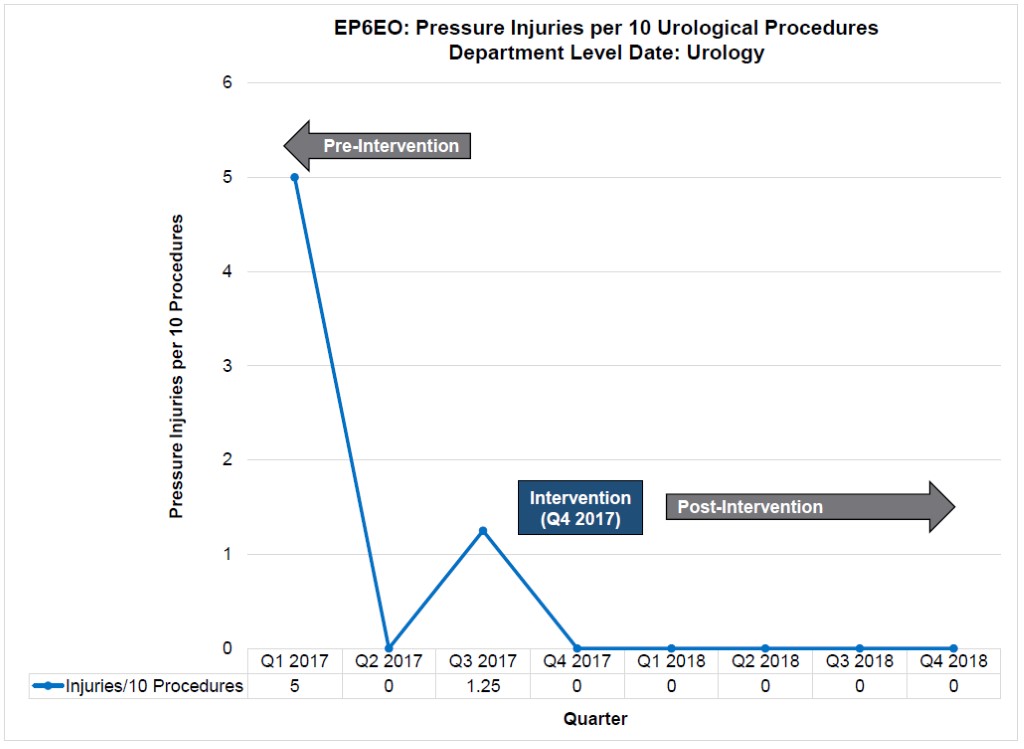
Back to 2019 Abstracts




