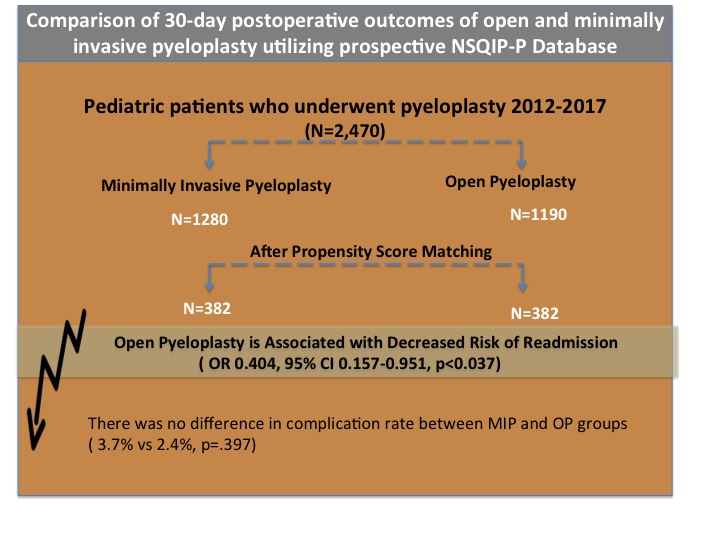
Comparison of 30 day postoperative outcomes of open and minimally invasive pyeloplasty utilizing prospective NSQIP-P database
Kimberly Woo, BS1, Laura Bukavina, MD MPH2, Kirtishri Mishra, MD2, Amr Mahran, MD MS3, Austin Fernstrum, MD2, Megan Prunty, MD2, Lee Ponsky, MD4, Heather DiCarlo, MD5, Jonathan Ross, MD2, Lynn Woo, MD2.
1Case Western Reserve School of Medicine, Cleveland, Ohio, Cleveland, OH, USA, 2University Hospitals Cleveland Medical Center/Rainbow Babies and Children's Hospital, Cleveland, OH, USA, 3University Hospitals Cleveland Medical Center, Cleveland, OH, USA, 4University Hospitals Cleveland Medical Center, Cleveland, Ohio/ Case Comprehensive Cancer Center, Cleveland, Ohio, Cleveland, OH, USA, 5Johns Hopkins School of Medicine/ The James Buchanan Brady Urological Institute, Baltimore, Maryland, Baltimore, MD, USA.
Objective To evaluate the differences in outcomes between minimally invasive pyeloplasty (MIP) and open pyeloplasty (OP) for the surgical correction of ureteropelvic junction obstruction in children.
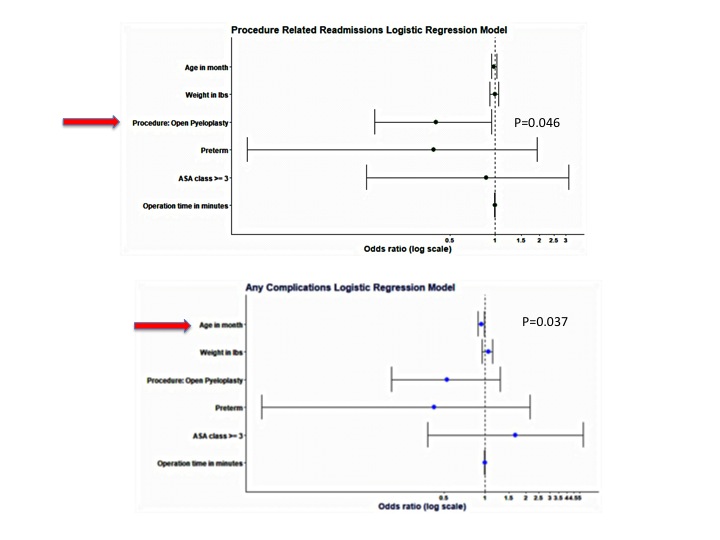
Methods Data was obtained from the pediatric National Surgical Quality Improvement Program (NSQIP) 2012-2017. We identified 1,280 patients who underwent MIP and 1,190 patients who underwent OP between and. Propensity score matching (PSM) was utilized to adjust for baseline differences. Univariate and multivariable regression were utilized to assess odds of complications and procedure related readmission.
Results Patients who underwent OP had a significantly decreased operative time (192.42 vs. 142.00 min, p < 0.001) compared to MIP. There was no significant difference in the rates of overall perioperative complications (3.7% (MIP) vs 2.4% (OP) p=0.397). On multivariable analysis, patients undergoing OP had a lower risk of procedure-related readmission (OR 0.404, 95% CI 0.157-0.951, p=0.046] than MIP. In a multivariable linear regression model, the risk of having any postoperative complication, regardless of surgical approach, decreased with increasing patient age [OR 0.945, 95% CI 0.893-0.996, p = 0.037].
Conclusion MIP offers a minimally invasive alternative to OP in the pediatric population with similar rates of perioperative complications. However, our study shows decreased odds of procedure related readmission in OP, which may serve as a surrogate for postoperative complications in these patients. 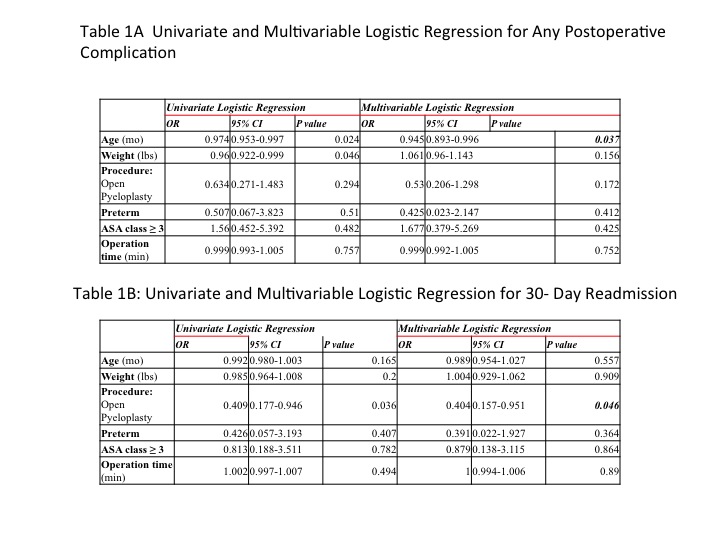
Back to 2019 Abstracts




