Development and validation of a scoring system for objective assessment of vesicoureteral reflux resolution using analysis and visualization of pre- and intraoperative factors of pediatric robot-assisted laparoscopic extravesical ureteral reimplantation: a multi-institutional internal and external validation analysis
Sang Hoon Song, MD., Ph.D.1, Il-Hwan A. Kim, Research Assistant1, Jae Hyun Han, MD., Ph.D.2, Kun Suk Kim, MD., Ph.D.2, Esther J. Kim, B.S.1, Kunj Sheth, M.D.1, Jonathan Gerber, M.D.1, Minki Baek, MD., Ph.D.3, Chester J. Koh, M.D.1.
1Division of Pediatric Urology, Department of Surgery, Texas Children's Hospital/Scott Department of Urology at Baylor College of Medicine, Houston, TX, USA, 2Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea, Republic of, 3Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of.
BACKGROUND: Robot-assisted laparoscopic extravesical ureteral reimplantation (RALUR-EV) has been reported as a viable minimally invasive surgical option for vesicoureteral reflux (VUR) with comparable success rates and complication rates to open reimplantation at several pediatric hospitals, but with lower success rates and higher complication rates at other centers, which may reflect technical or learning curve differences. We aimed to develop and validate a scoring system as an objective assessment tool for predicting VUR resolution after RALUR-EV.
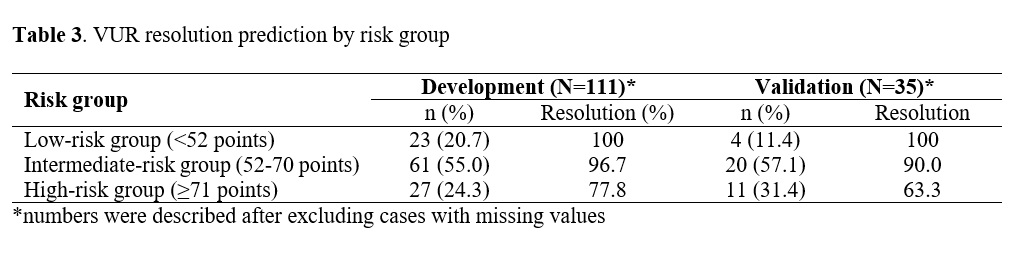
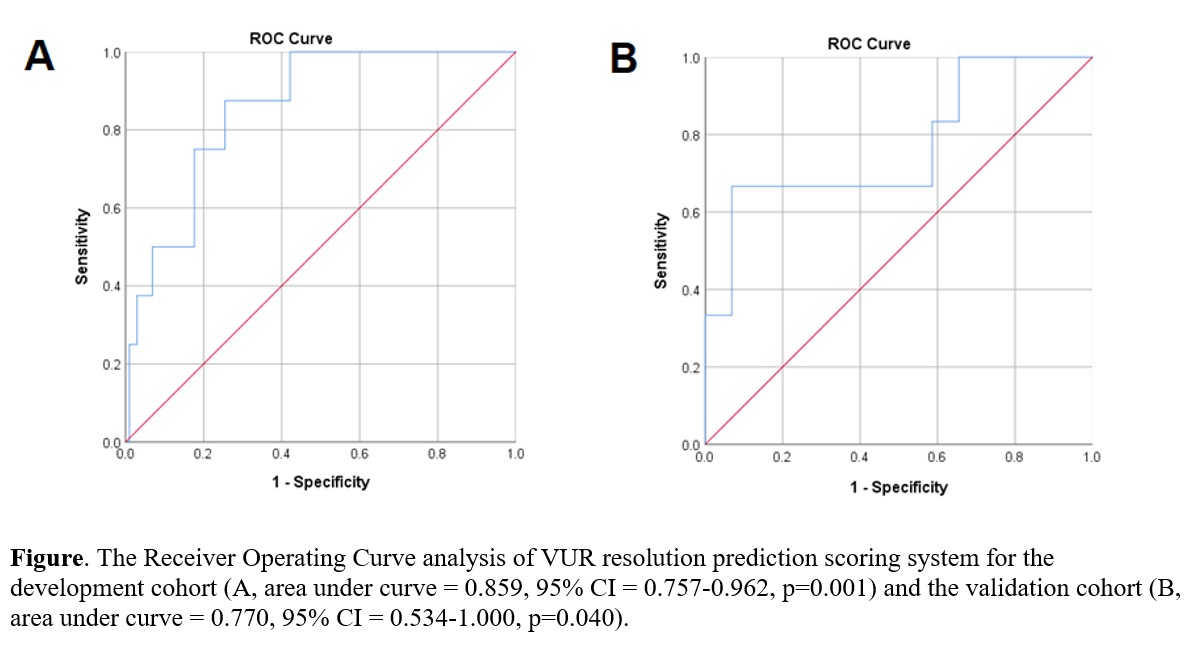
METHODS: Data for this multi-institutional retrospective cohort study of RALUR-EV patients was obtained from two tertiary referral hospitals. We utilized the admission values for age, sex, body mass index (BMI), bladder bowel dysfunction (BBD) status, VUR grade, console time, hospital stay and the number of detrusorrhaphy stitches as potential predictor candidates of VUR resolution. The larger cohort between the two institutions was designated as a development cohort and the other as an external validation cohort. We developed a logistic regression model for predicting VUR resolution. Patients were stratified into low, intermediate, and high-risk groups. External validation was performed using the model projected to the external validation cohort. RESULTS: 115 ureteral units in the development cohort and 46 ureteral units in the validation cohort were utilized for this study. The success rate of VUR resolution after RALUR-EV was 93.0% and 87.0% in the development and validation cohort, respectively (Table 1). For the VUR resolution score, the age, BMI, BBD, VUR grade, console time, and hospital stay were assigned to weighted points according to their β (regression coefficient) values based on the logistic regression analysis model (Table 2) as to be calculated as follows: age (yr) + BMI + BBD times 10 + VUR grade times 7 + console time (hr) + hospital stay times 6. The area under the Receiver Operating Characteristic (ROC) curve of our scoring system was 0.859 (p=0.001) and 0.770 (p=0.040) in the development and validation cohorts, respectively (Figure). VUR resolution was significantly different among risk groups: 100% (low-risk), 96.7% (intermediate-risk), and 77.8% (high-risk) (p=0.004) in the development cohort (Table 3). CONCLUSIONS: A novel VUR resolution scoring system using multiple pre- and intraoperative variables including patient's age, BMI, BBD, VUR grade, console time, and hospital stay provides a prediction of children at risk for failure of VUR resolution after RALUR-EV. 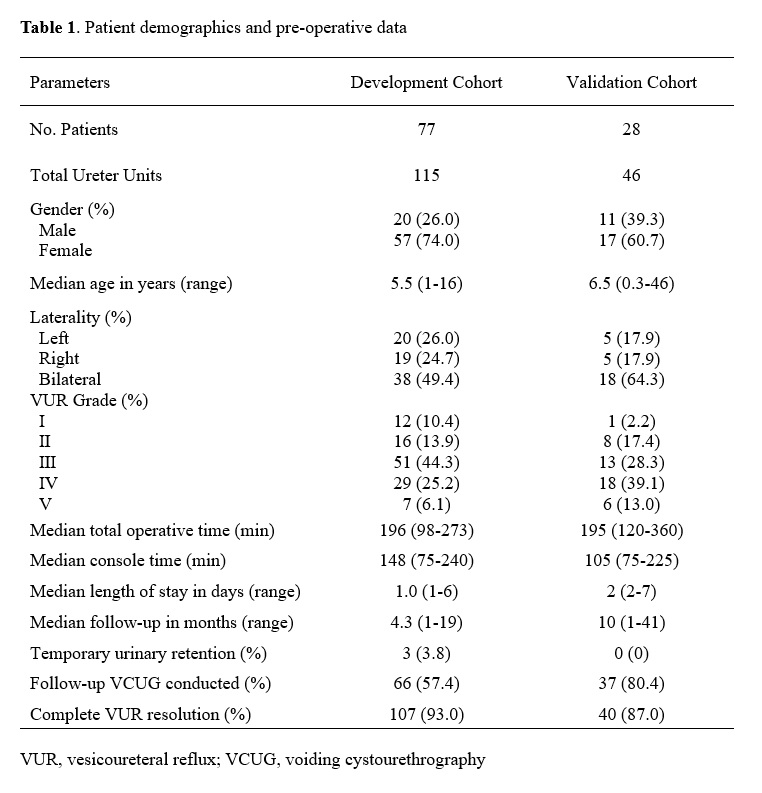

Back to 2019 Abstracts




