Urologic Imaging After Initial Febrile UTI in Primary Care Setting- The Current State
Hsin-Hsiao Scott Wang, MD, MPH, MBAn, Jonathan Hatoun, MD, MPH, Anudeep Mukkamala, MD, Laura Patane, BS, Louis Vernacchio, MD.
Boston Children's Hospital, Boston, MA, USA.
BACKGROUND: Timely imaging is recommended after febrile UTI (fUTI) in young children to identify treatable urologic conditions. The 2011 American Academy of Pediatrics (AAP) guideline recommends renal-bladder ultrasound (RBUS) after fUTI and voiding cystourethrogram (VCUG) after abnormal RBUS or second fUTI. Adherence to these recommendations by pediatric clinicians has not been characterized. We sought to investigate practice pattern variability and associated factors in pediatric fUTI imaging in primary care clinics.
METHODS: All children <24 months old with fUTI (temperature ≥38C, positive urinalysis, and >50,000 CFU on urine culture) in a large primary care network in Mass. in 2019 were reviewed. Those with congenital genitourinary anomalies were excluded. After bivariate analyses of potential covariates of age, gender, race, insurance, maximum temperature, setting (ER vs. office), presence of complex chronic conditions, practice size, and provider type and age, we fitted a multivariable logistic regression model with a primary outcome of adherence to the AAP guideline.
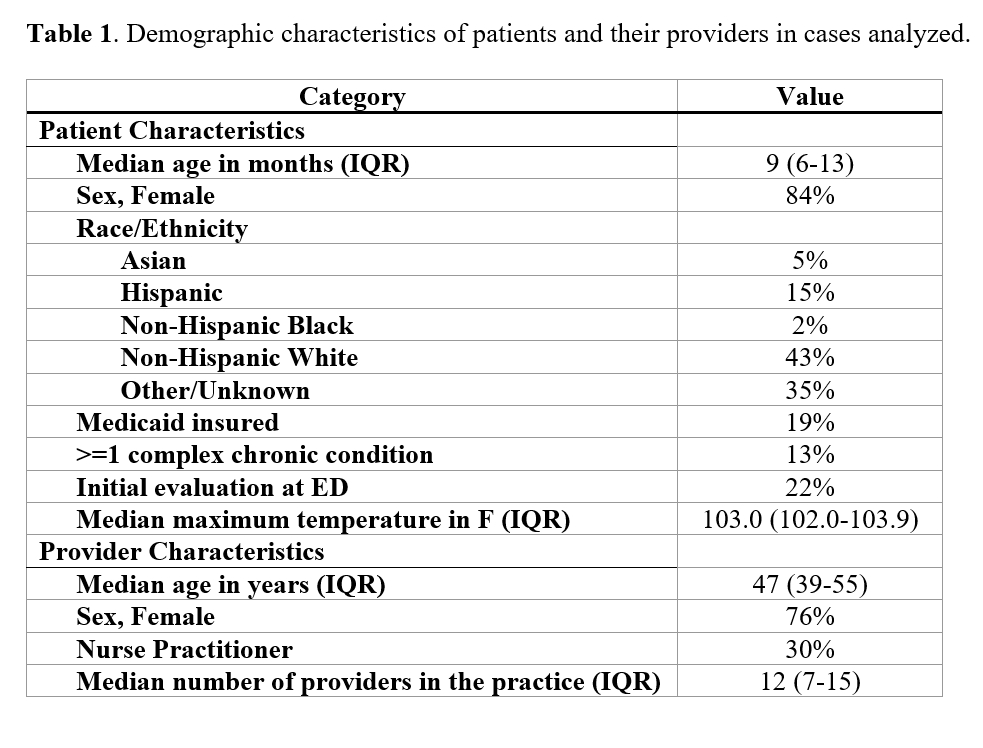
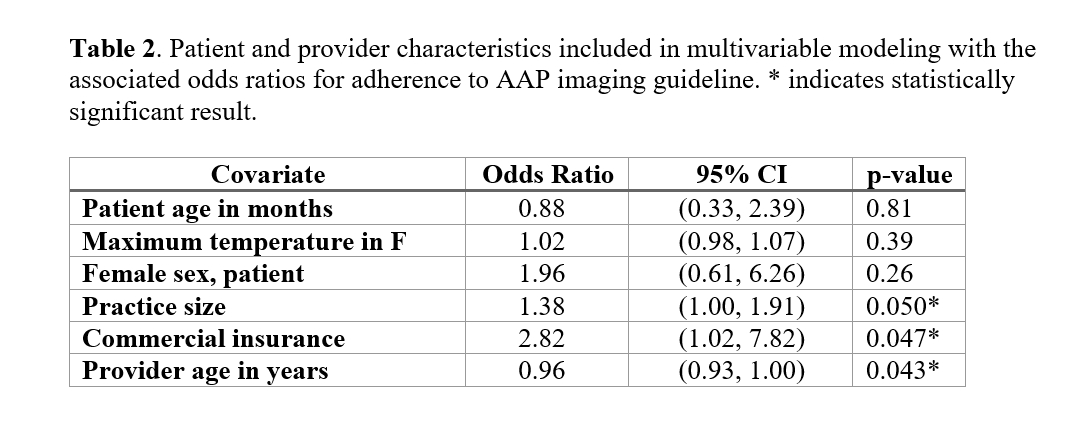
RESULTS: Table 1 shows the demographic characteristics of 118 patients with fUTI and their providers. Overall, post-UTI imaging was adherent to the AAP guideline in 82 cases (69.5%; Figure 1). Reasons for non-adherence were: no RBUS (N=21), VCUG despite normal RBUS (N=9), no VCUG after abnormal RBUS (N=4), and no VCUG after a second fUTI (N=2). In the multivariable logistic regression model (Table 2), significant predictors of guideline adherence were commercial insurance (OR=2.82, p=0.047), more providers in the practice (OR=1.38, p=0.05), and younger provider age (OR=0.96, p=0.043) after adjusting for patientís age, sex, maximal temperature during UTI.
CONCLUSION: Young children with fUTI received guideline-adherent imaging from their primary care clinician approximately 70% of the time in this sample, though significant opportunities for improvement exist. Errors of omission (not ordering a recommend study; 27/118 [23%]) and commission (ordering an unnecessary study; 9/118 [8%]) contributed to non-adherence. Guideline adherence was statistically more likely for commercially-insured patients, providers working in larger offices, and younger providers, suggesting both patient and provider characteristics impact the practice pattern. While the provider characteristics identified offer opportunities for training and clinical decision support, addressing the effect of insurance status on adherence may be more complicated. Since public insurance in this case may serve as a proxy for a multitude of other socio-economic factors, further quality improvement work is needed to understand how to increase the likelihood that patients with public insurance achieve guideline-recommended imaging after fUTI.

Back to 2023 Abstracts
