Comparison of incidence of urinary tract infections among patients with isolated hydronephrosis and primary megaureter: a risk-adjusted time-to-event analysis
Jin Kyu Kim, MD, Michael Chua, MD, MASc, Adree Khondker, BHSc, Kay Rivera, MD, Margarita Chancy, MD, Joana Dos Santos, MD, MHSc, Juliane Richter, MD, Armando Lorenzo, MD, MSc, Mandy Rickard, MN-NP.
The Hospital for Sick Children, Toronto, ON, Canada.
BACKGROUND: Primary non-refluxing megaureter (PM) is an entity that is separate from isolated hydronephrosis (HN). Literature has shown that patients with hydroureter are more likely to experience urinary tract infections (UTI) and have greater benefit from continuous antibiotic prophylaxis (CAP). While absolute risk reduction has been evaluated, there has been limited epidemiological assessment of time to UTI in a risk-adjusted manner. Herein, we combined the largest cohort of megaureter and isolated hydronephrosis reported in literature for a comparative analysis, using individualized patient data and time-varying exposure analysis.
Methods: Our institutional PM database, as well as isolated HN database were examined. PM defined as hydroureteronephrosis with dilatation > 7mm. We excluded patients with other etiologies for upper tract dilatation. UTI was defined as fever >38.5°C, with positive urinalysis and culture from catheterized specimens. Only UTIs within the first year of life were included. To adjust for time-varying exposure, patients were censored based on CAP discontinuation, UTI event, surgery, loss to follow-up, or hydroureter resolution. A Kaplan-Meier time-to-event analysis was performed.
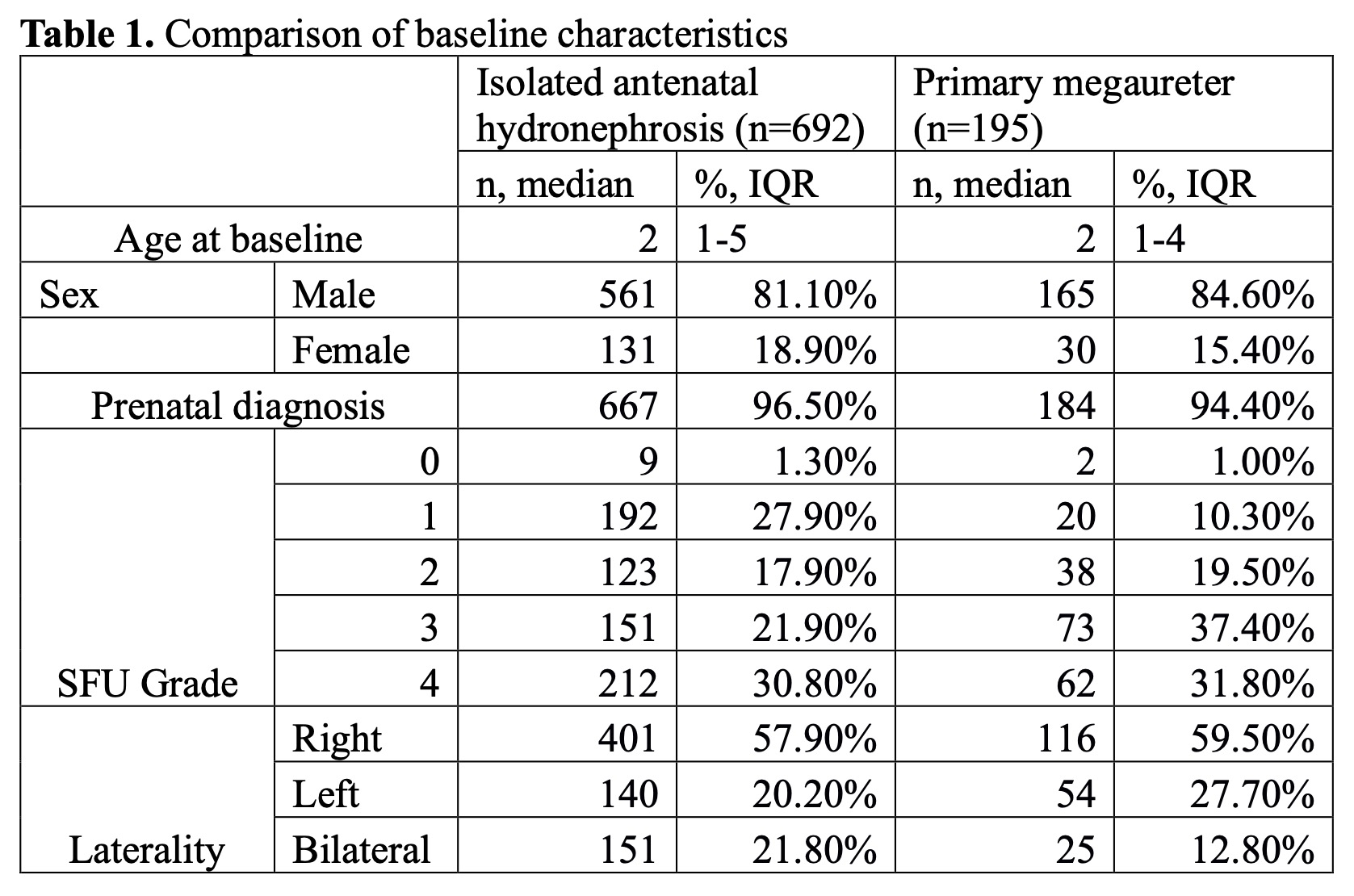
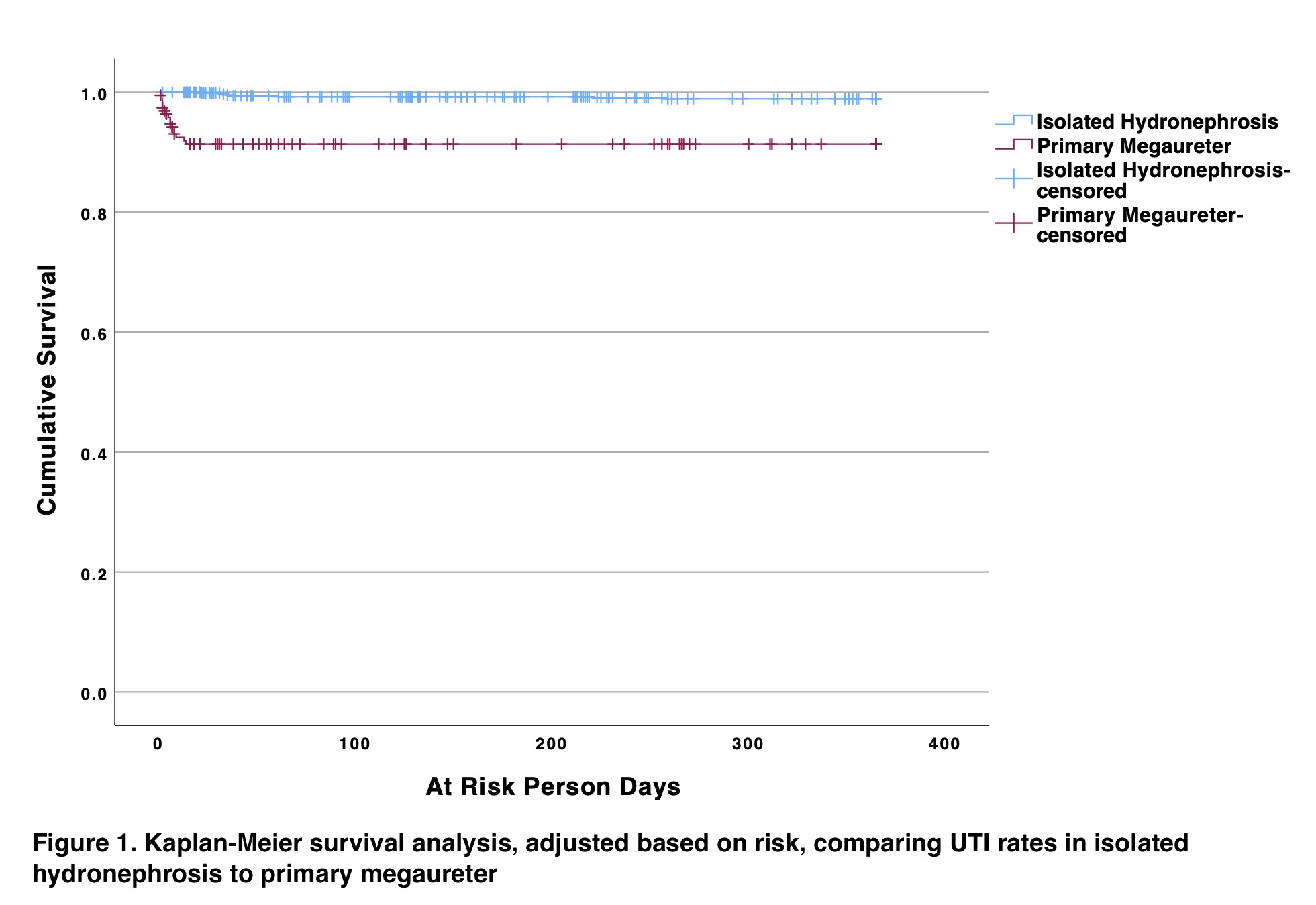
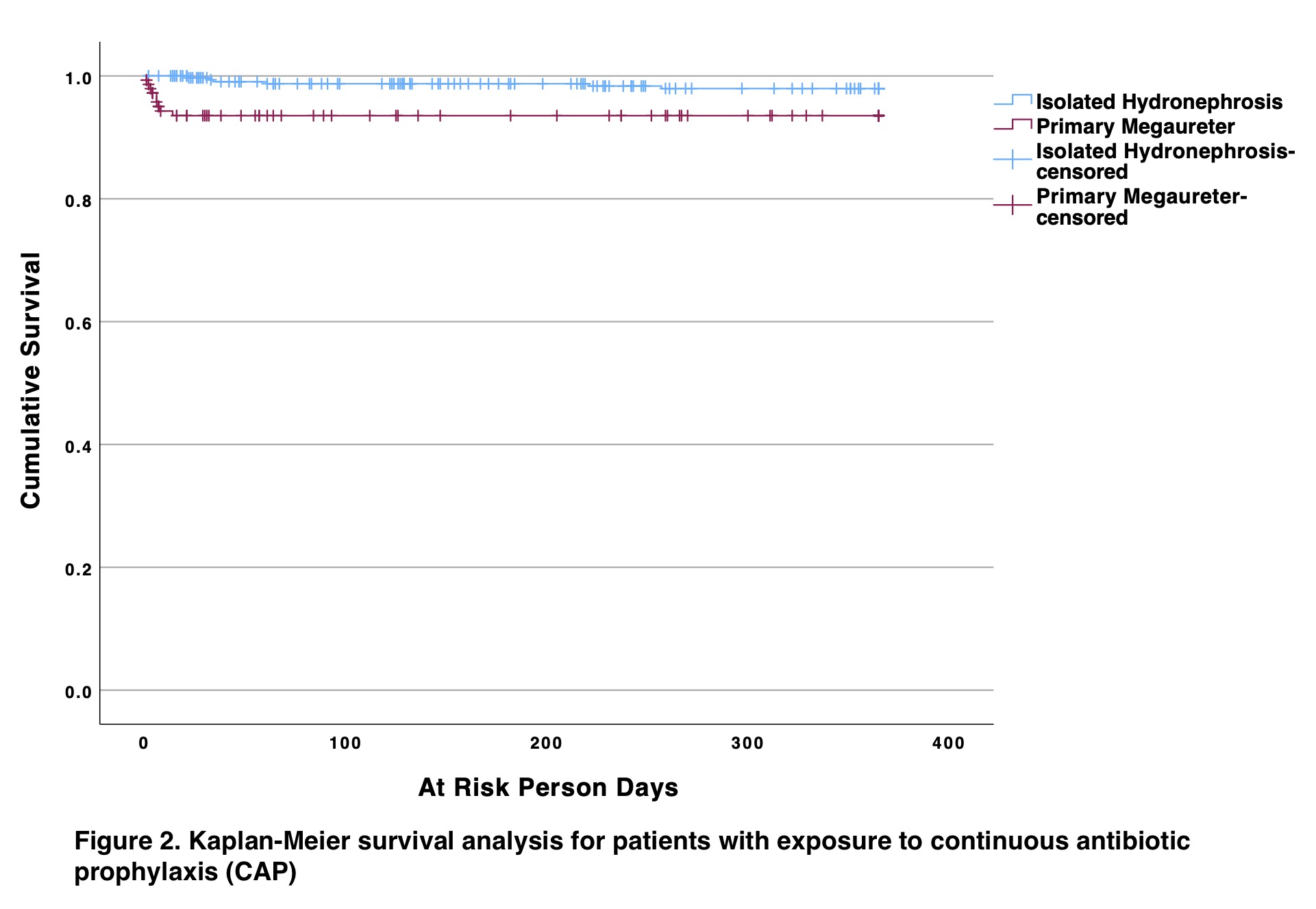
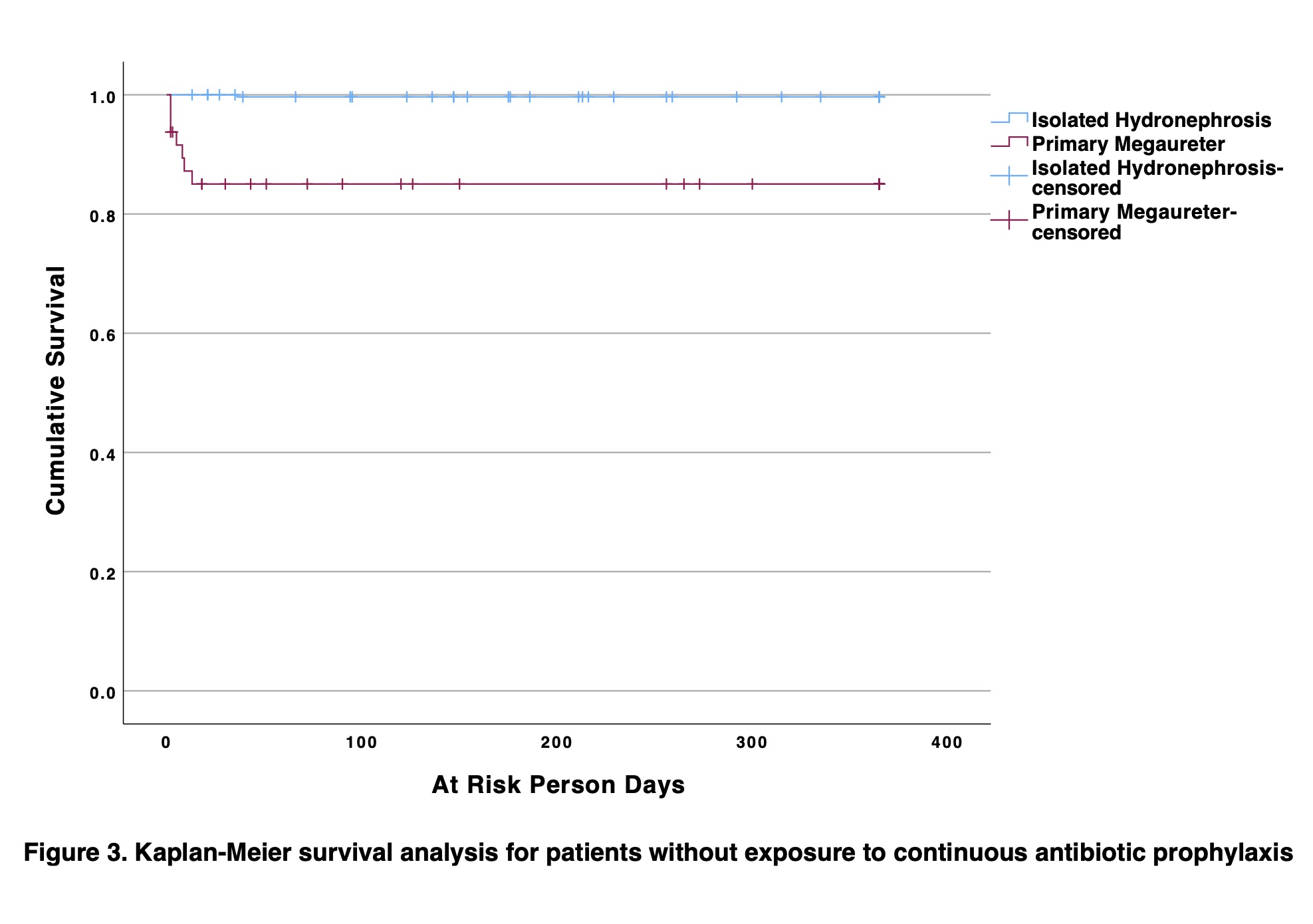
Results: A total of 195 patients with PM were identified and 692 patients with HN were identified. The baseline characteristics were similar across the three groups, including age at presentation, sex, antenatal diagnosis, laterality, and SFU grading (Table 1). Kaplan-Meier survival curve, accounting for time-varying exposure censoring, showed a clear split of the curve between those with PM and HN (Figure 1; log-rank p<0.001). When stratified by CAP exposure, CAP appeared to confer some protection for patients with PM with less divergent curves (Figure 2; log-rank p=0.006). In contrast, those without CAP exposure had a wider split of curves (Figure 3; p<0.001).
CONCLUSIONS:
The rates of clinically significant UTI are higher in patients with PM compared to those with isolated HN. While not statistically significant, CAP appears to have some protection for symptomatic UTIs for patients with PM and brings the survival curves closer to patients with isolated HN. While both represent upper tract dilations, isolated HN and PM should have different approaches to risk assessment for UTIs.
Back to 2023 Abstracts
