The Long-Term Effects of a Combined Video and Novel Simulation-Based Education on Undescended Testicle Diagnosis and Management on Pediatrician Comfort, Confidence, Skill, and Knowledge
Eric M. Bortnick, MD, Caleb P. Nelson, MD MPH.
Boston Childrens Hospital, Boston, MA, USA.
BACKGROUND: Pediatricians provide initial assessment and referral of boys with undescended testis (UDT) but receive little training in pediatric genitourinary physical exam (GUPE) and may not be familiar with UDT guidelines for management. We previously presented work showing an educational strategy combining asynchronous didactics and simulation-based learning improved pediatrician confidence, comfort, and skill performing the GUPE and increase knowledge on UDT management immediately after the education sessions. In this project, we assess the long-term impact of the education through a follow up survey.
Methods: We developed a novel manikin that permits realistic simulated GUPE for normal scrotal testicle, palpable UDT, nonpalpable UDT, and retractile testicle. Pediatricians (residents and attendings) participated in an educational session consisting of an asynchronous video on UDT guidelines and GUPE technique, followed by an in-person simulation session using the manikin. Participants were scored on GUPE technique and immediate deliberate feedback was performed until mastery was achieved. Three months after undergoing the education sessions, participants completed a follow up survey to assess comfort, confidence, knowledge, and practice changes.
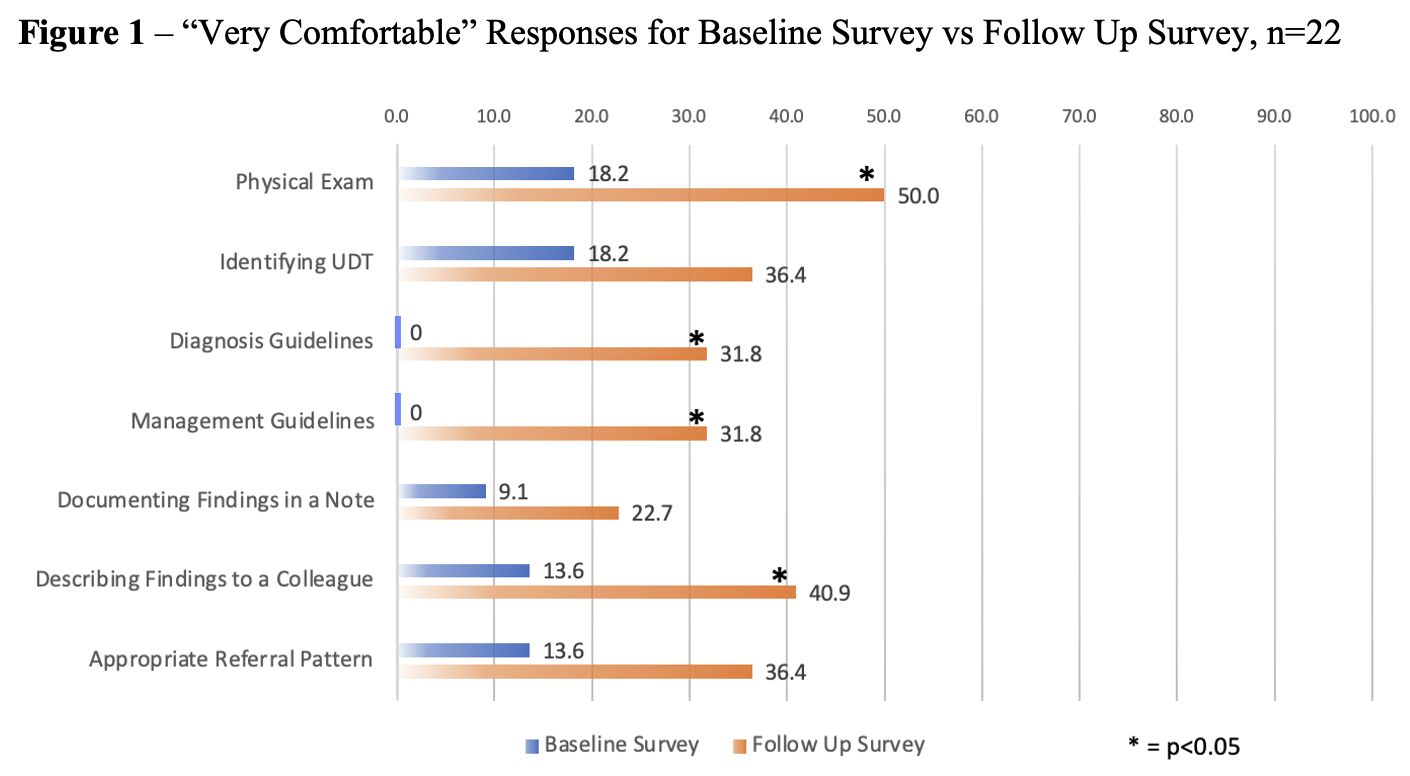
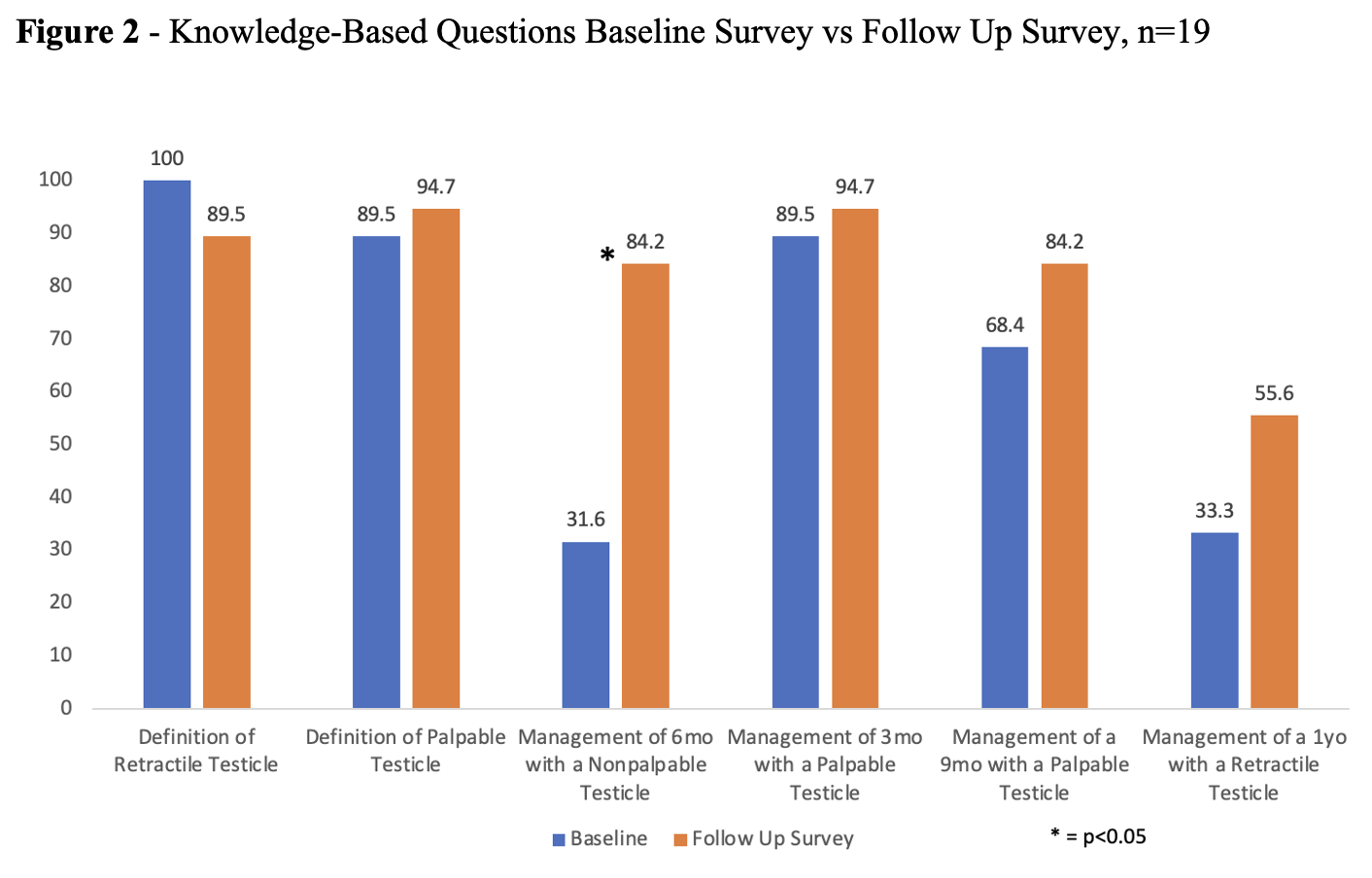
Results: 28 residents and 27 attendings completed the baseline survey, of whom 22 and 21 completed the simulation session. At baseline, only 22% were very comfortable in GUPE skill, 11% were very comfortable with identification of UDT, and none were very comfortable with UDT guidelines. 22 learners (13 residents and 9 attendings; 51.2% of education participants) completed the three-month follow up survey. Learners were asked the same comfort and confident questions as in the baseline survey. Learners responding feeling “very comfortable” more than doubled in every category, with statistically significant differences in physical exam performance, diagnosis and management guidelines, and describing physical exam findings to a colleague (Figure 1). 12/22 (54.5%) reported seeing a patient in clinic with concern for UDT in the three months since taking the education sessions. Of these, 91.7% reported modifying their GU physical exam technique, 41.7% reported changing the way they document GU physical exam findings, 33.3% reported referring patients with concern for UDT to a Pediatric Urologist at an earlier age, and 41.7% reported decreasing the number of ultrasounds ordered for UDT concerns. Learners improved on most board-style questions as compared to the baseline survey, with a significant difference in correct responses noted for the management of a 6-month-old with a nonpalpable testicle (Figure 2). CONCLUSIONS: Standardized education involving video and in-person simulation using a novel manikin has long-term effects in increasing confidence, comfort, physical exam skill, and UDT knowledge. Simulation with the novel manikin played a key role in the education. The educational strategy could be expanded to other institutions and extend to other provider types. Future studies may include quality improvement initiatives to study how participation can change patient outcomes.
Back to 2023 Abstracts
