Fertility preservation amongst transgender girls in a multidisciplinary gender affirmation program
Alexandra R. Siegal, MD1, Nir Tomer, MD1, Eva M. Baldisserotto, CPNP-PC2, Erin Miller, CPNP-PC2, Mabel Yau, MD3, Matthew Oransky, MD4, Joshua D. Safer, MD4, Fernando A. Ferrer, MD2, Neha R. Malhotra, MD3.
1Icahn School of Medicine at Mount Sinai, New York, NY, USA, 2Mount Sinai Kravis Children’s Hospital, New York, NY, USA, 3Mount Sinai Kravis Children’s Hospital and Center for Transgender Medicine and Surgery, New York, NY, USA, 4Mount Sinai Center for Transgender Medicine and Surgery, New York, NY, USA.
BACKGROUND: Transgender and gender diverse people initiating gender affirming hormonal therapy or puberty blockade may experience an impact on reproductive ability. Discussion of fertility preservation (FP) is therefore an important step in the decision making for patients seeking gender affirming care. The first aim of this study was to understand the overall proportion of transgender girls who pursued fertility preservation in a practice where a pediatric urology team is integrated into a multidisciplinary transgender medicine and surgery program. The second aim was to assess the quality of semen for those who completed cryopreservation.
Methods: A retrospective review of transgender and gender diverse patients 21 years or younger with testes who sought gender affirming care was performed. The study period was between April 2022 and April 2023, the first year following integration of pediatric urology into the multidisciplinary program. Demographics, age, hormonal treatment, Tanner stages, FP outcomes, and semen analysis were recorded.
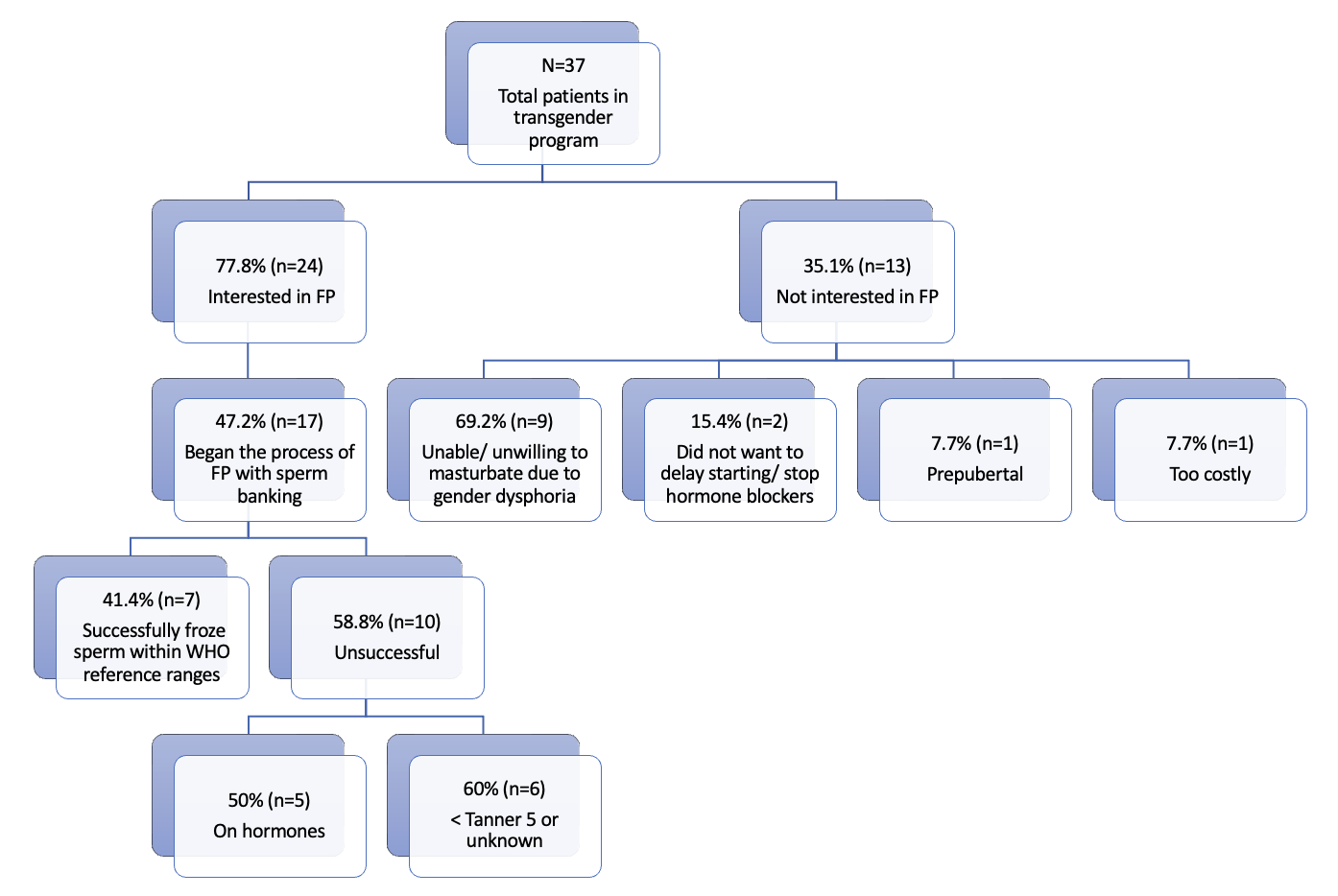
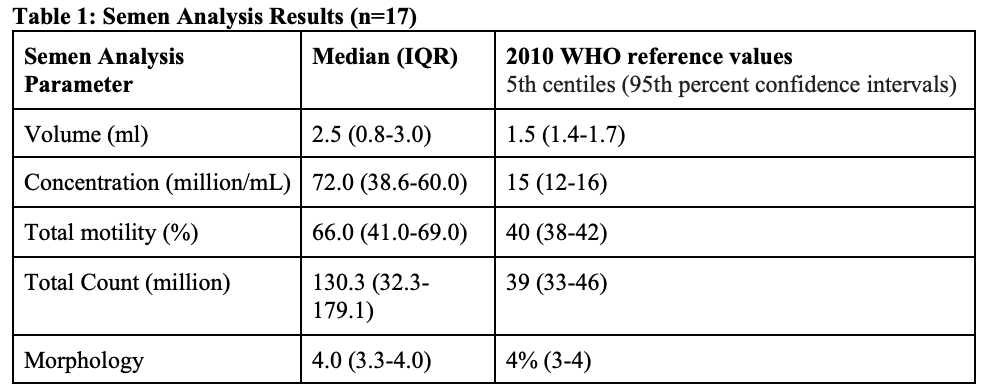
Results: 37 patients with a mean age of 15.1 +/- 1.9 years met inclusion criteria. As described in Figure 1, 77.8% (n=24) were interested in pursuing/are in the process of sperm banking. Of the patients who did not pursue FP (n=12), 69.2% (n=9) reported unwillingness or inability to masturbate due to gender dysphoria, 15.4% (n=2) did not want to delay starting or stop hormone blockers, 7.7% (n=1) were prepubertal (Tanner I), and 7.7% (n=1) cited sperm banking as too costly. 47.2% (n=17) of patients began the process of FP with sperm banking, seven (41.4%) of whom had successful cryopreservation within WHO reference ranges of semen parameters. Of the children who did not meet WHO criteria, half were on hormone medications (50%, n=5). One child had azoospermia; upon review, it was found that they already started hormonal suppression. Average results of semen analysis are presented in Table 1.
Conclusions: Fertility preservation (FP) is an important step prior to initiating gender affirming hormonal therapy or puberty blockade. Data suggest that with the integration of a pediatric urology team, a high percentage (78%) of patients may be interested in fertility preservation. Nearly half of patients began the process of FP with sperm banking, 41% of whom successfully froze sperm within WHO reference ranges of semen parameters. These rates are high compared to previous studies regarding interest in pursuing and completing fertility preservation in transgender females (47-62% and 8.6-17%, respectively). Our findings highlight the importance of the integration of pediatric urology and FP into the health care process prior to pubertal suppression therapy.
Back to 2023 Abstracts
