Maximizing complication and near miss reporting in pediatric urology morbidity and mortality conference: a quality improvement initiative
Amanda Raines, MD, Ronelle Caskey, ARNP, Paul Merguerian, MD.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: Morbidity and mortality conference (M&M) provides a safe space for health care providers to discuss complications and near misses with the goal of improving quality of care. To achieve this goal, it is important to maximize reporting of complications and near misses. We aimed to improve complication reporting in our divisional pediatric urology M&M with the hypothesis that we could implement use of an automated system linked to our electronic medical record to capture 100% of complications and near misses.
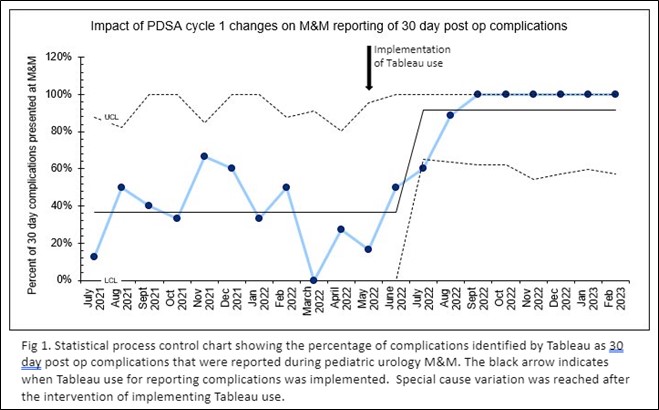
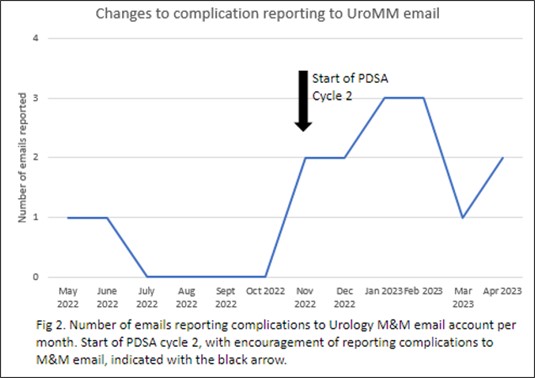
Methods: This was a single institution multiphase quality improvement project. We performed a current state analysis of pediatric urology M&M reporting and found that we were consistently not reporting all complications within the 30 day post operative period, particularly emergency room visits when patients were discharged. In PDSA (Plan Do Study Act) cycle 1, we used Tableau (Seattle) an automated analytic software linked to the electronic medical record to capture 30 day post-operative complications. Tableau was structured to report return to the operating room, return to the emergency department, and readmission within 30 days of surgery. Five month after instituting this intervention we studied our results and found that some complications and near misses were not reported. As a result, we implemented a PDSA cycle 2 which focused on improving reporting of complications and near misses by staff through a dedicated M&M email.
Results: Prior to the intervention, reporting of 30 day post operative complications ranged from 0-66%. After implementing PDSA cycles 1 and 2 over a period of 4 months the 30 day post operative complication reporting increased to 100% and was maintained at 100% for 6 months (Figure 1). During the study phase of PDSA cycle 1, we found that while reporting of 30 day post operative complications from Tableau improved, we were still missing some complications and near misses that did not meet the Tableau criteria. After encouraging reporting of complications to a dedicated M&M email, number of emails reporting complications improved from a median of 0 during PDSA cycle 1 to a median of 2 during PDSA cycle 2 (Figure 2). CONCLUSIONS:
Implementing an automated system to capture 30 day post operative complications improved reporting of complications and near misses. We found out, however, that utilization of an automated system alone is not enough and reporting of complications and near misses by staff and providers is necessary in order to capture all complications and near misses.
Back to 2023 Abstracts
