Adults with Spina Bifida Fare Worse than Young Adults: A Novel Systemic Vulnerability in Urinary Tract Infection-Related Hospital Care
Kathy Huen, MD, MPH1, Carol Davis-Dao, PhD2, Lois Sayrs, PhD2, Louis Ehwerhemuepha, PhD2, Chloe Martin-King, PhD2, Zeev Kain, MD2.
1UCLA, Los Angeles, CA, USA, 2Children's Hospital of Orange County, Orange, CA, USA.
BACKGROUND: Previous studies exploring the impact of age on healthcare utilization in individuals with spina bifida (SB) have typically focused on the comparison of adolescents (<18 years) to young adults (YA, 18-25 years). Using a large, nationwide clinical database, we aim to estimate the risks of urinary tract infection (UTI)-related emergency department (ED) visits and inpatient admissions (IP) as SB patients transition from adolescence to adulthood, beyond 25 years of age.
METHODS: Using Cerner Real World Data (CRWD), a database composed of data from over 100 health systems in the United States, we conducted a retrospective cohort analysis comparing SB patients to an age- and gender-matched cohort of non-SB patients without complex chronic conditions for ED and IP UTI-related encounters. SB cases from 2015-2021 were identified, excluding anencephaly and SB occulta. Patients aged 11-35 years were captured and compared in 3 cohorts: 11 to 17 years (adolescents), 18 to 25 years (YA), and 26 to 34 years (adults). Descriptive statistics were compared using chi-square and pairwise Wilcoxon rank sum tests. Logistic regression was performed to characterize the risk of healthcare utilization associated with transitioning from pediatric to adult care.
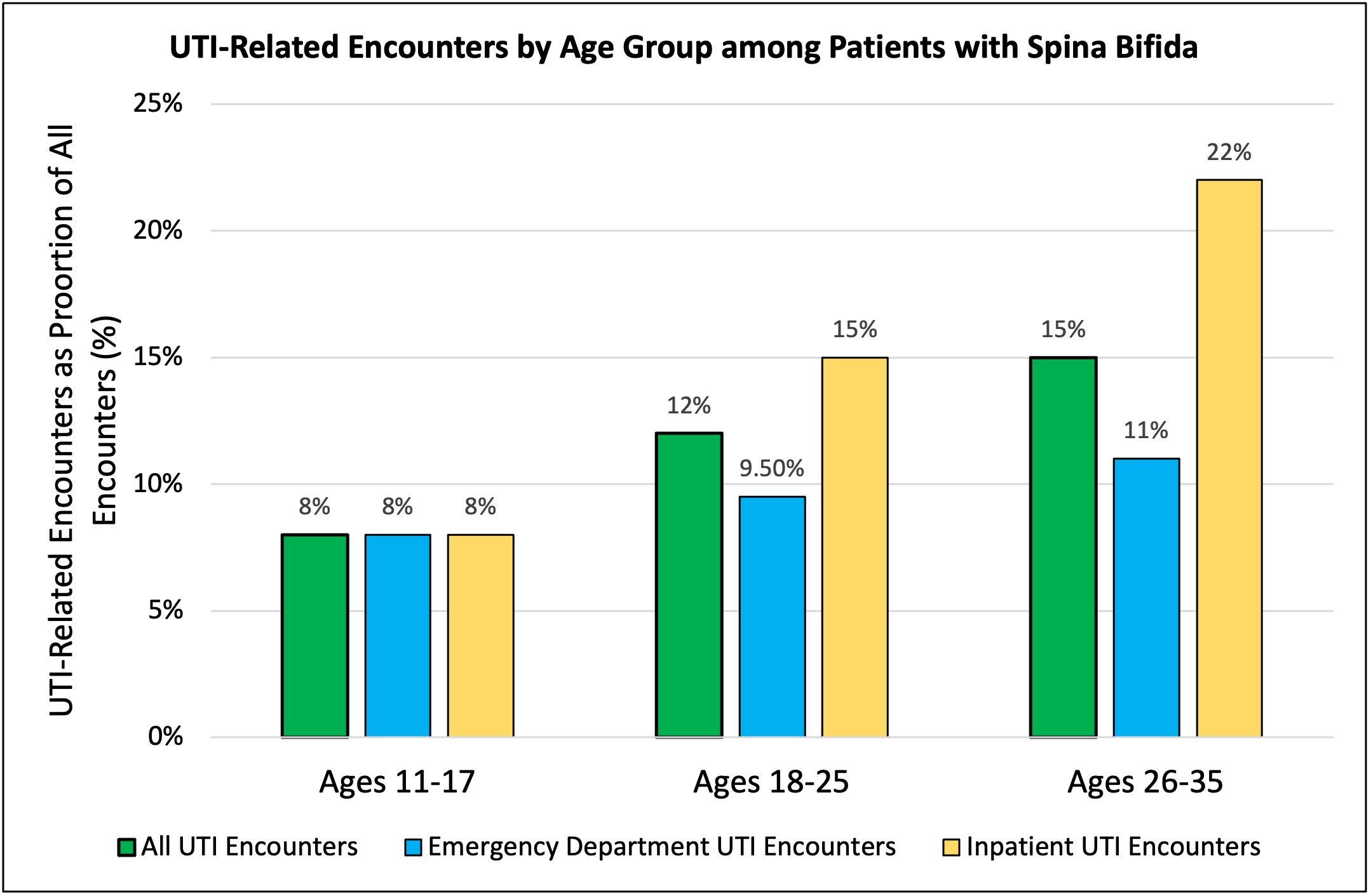
RESULTS: Of the 8,347 patients with SB and 150,988 non-SB controls identified, 2164 SB patients (26%) and 4832 of controls (3%) had at least 1 UTI encounter. UTI-related encounters as a proportion of all encounters significantly increased with increasing age in SB patients (adolescents 8%, YA 12%, adult 15%, p<0.0001). The proportional increase was more prominent in the IP setting as compared to the ED setting. In the control group, UTI-related encounters as a proportion of all encounters increased with the transition of adolescents to YAs, but remained the same from YA to adults (adolescents 1.0%, YA 2.0%, adults 2.0%, p<0.0001). In adults, UTI-related encounters were significantly more likely to be associated with public insurance (adolescents 54%, YA 66%, adult 72%, p<0.0001). In SB patients with at least 1 UTI encounter, the median UTI encounters per individual was significantly higher in adults (2.0 UTI encounters, IQR 1-3), as compared to adolescents and YA (1.0 (IQR 1-3), p< 0.0001; 1.0 (IQR 1-3), p = 0.0002; respectively). Adjusting for race, sex, insurance type and comorbidities, the odds of visiting the ED or being admitted as an IP for UTI as an adult >26 years was 1.5 times higher than adolescents and YA (adjusted odds ratio 1.44, 95% CI 1.35-1.54, p<0.0001).
CONCLUSIONS: The odds of UTI-related hospital care were significantly higher in adults with SB over 26 years of age as compared to adolescents and YA. Identifying factors affecting transitional urological care beyond young adulthood merits further exploration.
Back to 2023 Abstracts
