Shared Decision Making in DSD: Bridging Family-Centered Care and Advocacy
David E. Sandberg, PhD1, Sophie Lightfoot, PhD (c)2, Meg Carley, B.Sc3, William Brinkman, MD, MEd, MSc4, Melissa Gardner, MA1, Larry D. Gruppen, PhD1, Noi Liang, BA, MBA5, Kendra Pinkelman, BA6, Phyllis W. Speiser, MD7, Kristina I. Suorsa-Johnson, PhD8, Brian A. VanderBrink, MD4, Jessica Wisniewski, BSc9, Dawn Stacey, RN, PhD, FCAHS, FAAN, FCAN, CON(C)2.
1University of Michigan Medical School, Ann Arbor, MI, USA, 2University of Ottawa, Ottawa, ON, Canada, 3Ottawa Hospital Research Institute, Ottawa, ON, Canada, 4Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA, 5Patient advocate, Denver, MI, USA, 6Parent advocate, Toledo, OH, USA, 7Donald and Barbara Zucker School of Medicine at Hofstra, Hempstead, NY, USA, 8University of Utah Spencer Fox Eccles School of Medicine, Salt Lake City, UT, USA, 9Parent advocate, Ann Arbor, MI, USA. Background. Few topics in pediatrics are as controversial as the management of disorders/differences of sex development (DSD). These conditions can be associated with increased risks of gonadal tumors, hypogonadism, infertility, gender dysphoria, psychosocial/sexual distress, and pervasive challenges for patients and their families. Among the most contentious decisions are consideration of genital and/or gonadal surgery.
Evidence of disputes over clinical management appears in the medical literature, social media, and debates in legislatures. Activists claim that clinicians bias parents’ healthcare decisions in directions preferred by the provider. This circumstance fuels the argument that proxy decisions made by parents, some irreversible, are a violation of the child’s human rights.
To address concerns that parents are making poorly informed decisions with tacit encouragement of clinicians, we developed decision aids for parents to engage as partners in proxy shared decision making (SDM) on behalf of young children. Considered the crux of patient and family-centered care, SDM is a collaborative process allowing patients and clinicians to make healthcare decisions together taking into account the best available evidence and patients’ (or their proxies’) weighted values and preferences for particular outcomes. Patient decision aids (PtDAs) support SDM by making decisions explicit, providing information about options and associated benefits/harms in a nontechnical and accessible manner, and helping clarify congruence between the chosen option and patient/family values.
Methods. The research team included 4 pediatric clinicians (psychologist, general pediatrician, pediatric endocrinologist, and urologist), 2 parents of young children with DSD, an adult with DSD, and PtDA design experts. PtDA development followed a co-design process, guided by the Ottawa Decision Support Framework and the International Patient Decision Aids Standards (IPDAS). A survey of clinicians delivering pediatric DSD care (n=28) identified 4 priority needs and created PtDAs for each – diagnostic exome sequencing; gender of rearing; and surgery (gonadal and genital). Alpha testing to determine the comprehensibility, usability, and acceptability followed. This presentation focuses on the 2 surgical PtDAs.
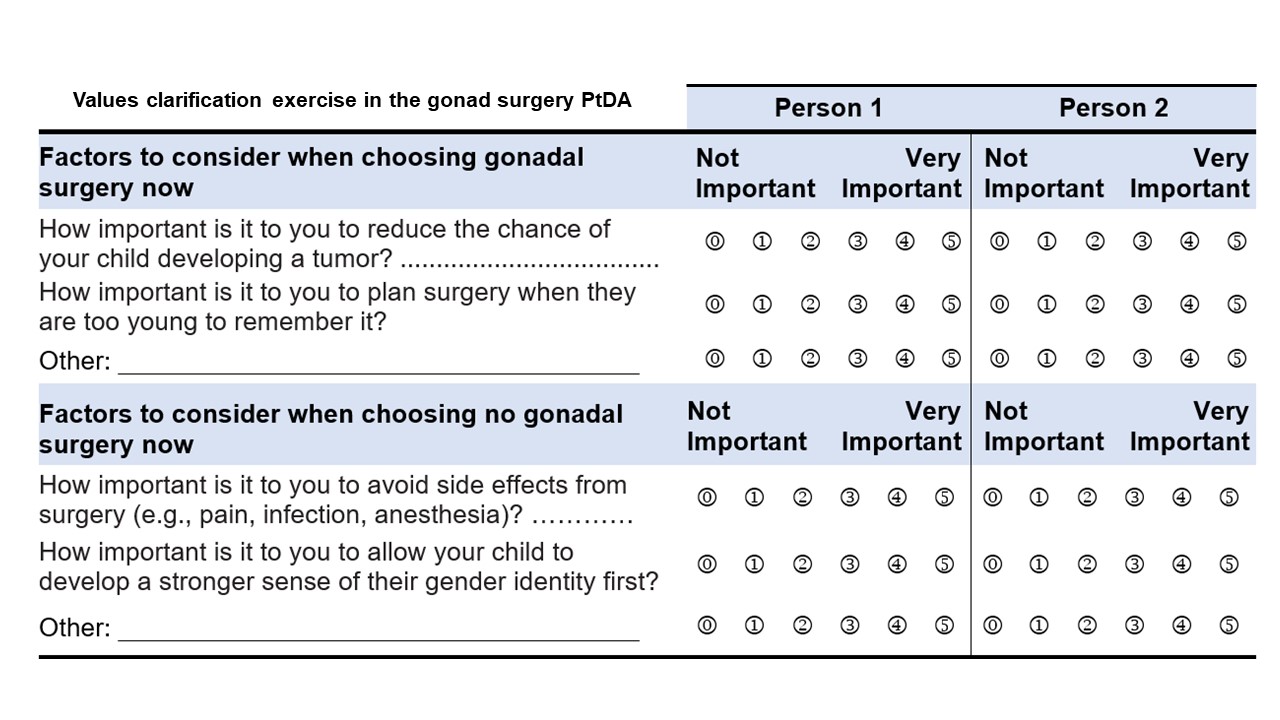
Results. Plain language information on the condition, available options, benefits and harms are presented in a format facilitating comparison between the positive and negative features of options with linkages to evidence sources, including expert opinion or consensus and with attention to ethical considerations. The PtDAs provide an interactive exercise to clarify parents’ values for features of options by using a 6-point scale (see Table). Alpha testing contributed to iterative changes in language and format which improved understandability and reduced perceptions of bias in presentation.
Conclusions. Although not directly responding to the charge that elective genital or gonadal surgery violates the child’s bodily autonomy, proxy PtDAs operationalize the ethical standard of informed decision making. If practiced with fidelity, this approach represents an alternative to legislative injunctions which fail to consider the patient and family in front of us. Next steps include evaluating factors influencing implementation of all 4 PtDAs in routine clinical practice and assessment of parents’ decisional outcomes.
Back to 2023 Abstracts
