Prior DVIU is Not a Poor Prognostic Factor for Urethroplasty Success in Pediatric Patients
Michael Pintauro, MD1, Avinash Maganty, MD2, Valentina Grajales, MD3, Paul Rusilko, DO1, Rajeev Chaudhry, MD4, Omar Ayyash, MD4.
1UPMC, Pittsburgh, PA, USA, 2University of Michigan, Ann Arbor, MI, USA, 3MD Anderson Cancer Center, Houston, TX, USA, 4Children's Hospital of Pittsburgh, Pittsburgh, PA, USA.
BACKGROUND:Pediatric urethral stricture disease is uncommon but can have a significant impact on a child’s life. Surgical management is akin to that of adults, with mainstays including urethroplasty and direct vision internal urethrotomy (DVIU). Although both are utilized successfully, urethroplasty has become more common and has a higher documented success rate as compared to DVIU. We sought to evaluate if DVIU prior to urethroplasty impacted surgical outcomes.
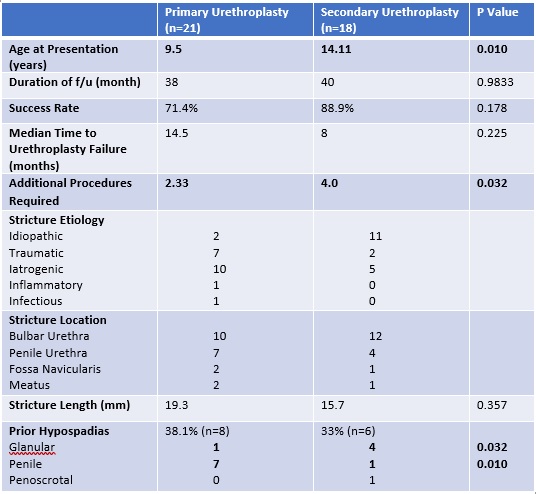
Methods: We retrospectively reviewed all patients at a single institution who underwent treatment of a urethral stricture between 2005-2020. Patients with less than one year of follow up were excluded. The primary outcome was recurrence rate for initial urethroplasty (primary group) versus post-DVIU urethroplasty (secondary group). Secondary outcomes included trends in surgical techniques and stricture characteristics such as etiology, location, and length.
Results: A total of 49 patients underwent either primary urethroplasty or secondary urethroplasty as treatment of their urethral stricture disease. Patients who underwent primary urethroplasty were significantly younger than those who underwent secondary urethroplasty (Table 1, p<0.05). There was no significant difference in success rates, overall rates of hypospadias, stricture length, stricture location. Both groups had high rates of traumatic etiology of stricture (47.6% and 27.8% for primary and secondary urethroplasty groups, respectively). Interestingly, the primary urethroplasty group had a significantly greater number of patients with prior penile hypospadias repair than the secondary group (87.5% vs. 16.6%, p<0.05), whereas the secondary group had significantly greater rates of glanular hypospadias (12.5% vs. 66.6%, p<0.05). Finally, patients with stricture recurrence after urethroplasty post-DVIU required more additional procedures as compared to those who failed primary urethroplasties (p=0.03). There were no procedural complications for DVIU. CONCLUSIONS: Patients who undergo DVIU prior to urethroplasty are not at higher risk of treatment failure if they undergo a future urethroplasty for the same stricture. Given its minimally invasive nature and low complication rate, DVIU is still a reasonable option for patients to trial prior to pursuing urethroplasty.
Back to 2023 Abstracts
