One and Done: Feasibility and Safety of Primary Ureteroscopy in a Pediatric Population
Paul Campbell, DO1, Brandon Mudd, MD2, Kiersten Craig, MD, MSE1, Michael Daugherty, MD, MHI1, Brian Vanderbrink, MD1, William DeFoor, MD, MPH1, Eugene Minevich, MD1, Pramod Reddy, MD1, Andrew Strine, MD, MPH1.
1Cincinnati Children's Hospital, Cincinnati, OH, USA, 2Univeristy of Cincinnati Urology, Cincinnati, OH, USA.
Background:
Pediatric urolithiasis has been increasing at rate of 4-10% annually in the United States, most notably within the adolescent and female population. Even with the increased use of medical expulsive therapy, a significant number of children will require surgical management of their stones. Primary ureteroscopy (URS) affords the opportunity to treat stones under a single anesthetic with lower re-treatment rates and anatomical or stone characteristic limitations compared to extracorporeal shockwave lithotripsy. Previous studies evaluating primary URS have been largely underpowered, are limited by stone location, and are not representative of the stone population seen in our demographic today. We sought to evaluate the success rate of primary URS and patient characteristics predicative of a favorable outcome at a tertiary referral center in the United States.
Methods:
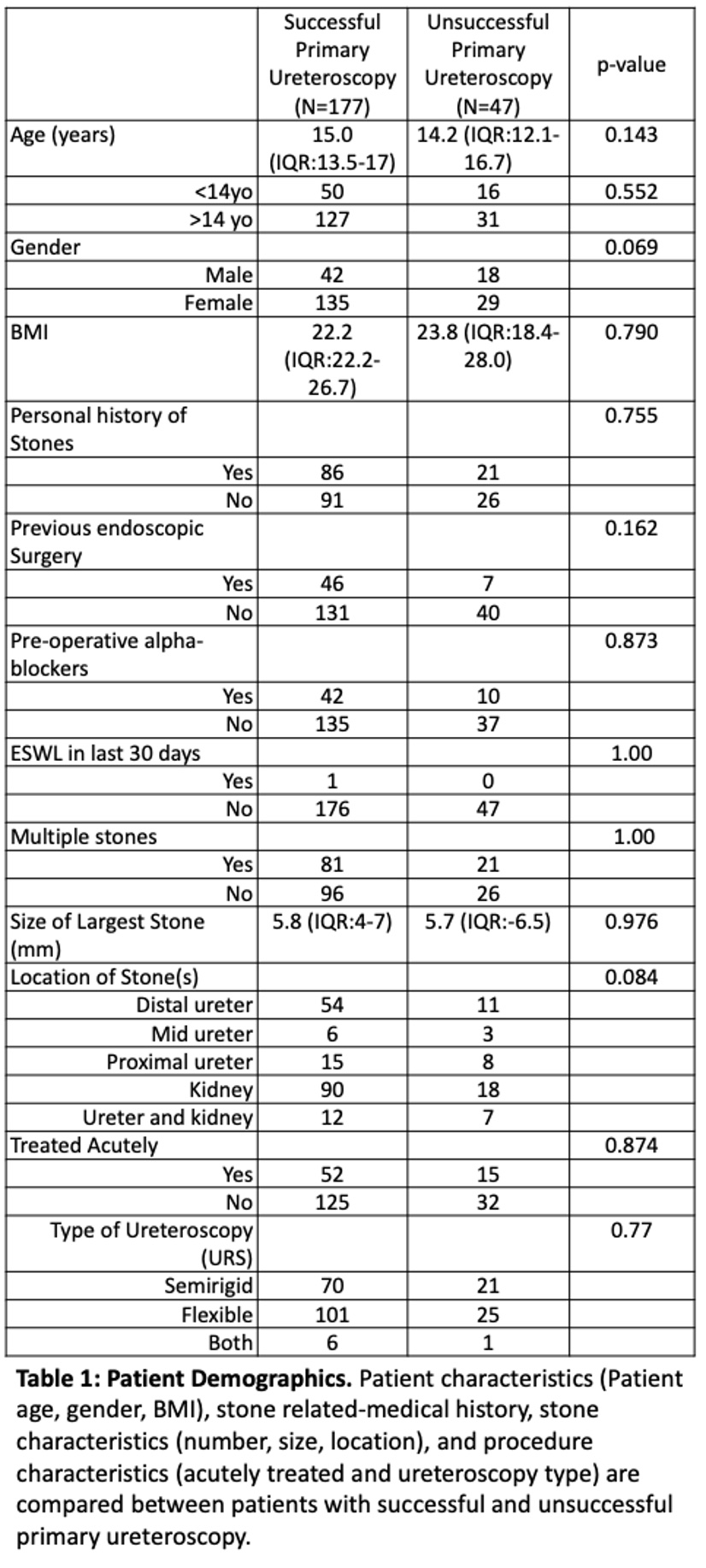
We conducted a retrospective cohort study of pediatric patients less than 18 years of age who underwent primary URS due to urolithiasis between 2011-2023. Patients were excluded if they were greater than 18 years old, had a previously placed stent to allow for passive ureteral dilation prior to URS, or if diagnostic URS was performed. A primary URS was considered successful if access to the ureter was obtained and treatment of the stone(s) completed. If unable to access the ureter, a stent was placed for staged URS. The primary outcome was success rate and patient characteristics predictive of a success. Secondary outcomes included the clinical stone free rates (SFR), 30-day emergency department (ED) visits, 30-day unplanned readmissions, and complications.
Results:
A total of 217 patients met inclusion criteria and primary URS was performed or attempted on 224 renal units (RU). The median age was 15.8 (IQR 13.4-16.9) years, and the median follow up was 8.4 (IQR 1.1-24.6) months. The success rate of primary URS was 79% (177/224 RU). There were no significant differences between successful and unsuccessful primary URS, including: age (<14 years vs. > 14 years, p=0.55), sex (p=0.07), BMI (p=0.79), history of stones (p=0.75), history of endourologic procedures (p=0.16), preoperative alpha antagonist (p=0.87), location of stone(s) (p=0.084), presence of multiple stones (p=1.00), type of URS performed (p=0.77), or treatment in the setting of admission due to acute renal colic (p=0.87). With successful primary URS, the SFR was 88% with larger stone size (p=0.001) being the only predictor of having residual stones. The 30-day ED rate was 19.6%, 30-day unplanned readmission rate was 11.6%, and overall complication rate was 7.5%. No Clavien-Dindo grade 4-5 complications or ureteral strictures occurred.
Conclusions:
To our knowledge, this is the largest study evaluating primary URS in the pediatric population in the United States. Primary URS can be completed safely in the majority of patients without any predictors of success. We advocate for primary URS when possible due to the excellent SFR and potential of treating stones under a single anesthetic.
Back to 2023 Abstracts
