Analysis of Clinical Characteristics and Surgical Management in Pediatric Patients with Ureteroceles in the SPU Hydronephrosis Taskforce
Shannon Cannon, MD1, Carol A. Davis-Dao, PhD2, Rebecca S. Zee, MD, PhD3, Sarah H. Williamson, MD4, Melissa McGrath, BASc5, Vishnu Sridhar, BS1, Jennika L. Finup, NP1, Rocio Goodman, BS1, Gabrielle A. Grob, BA3, Valre W. Welch, NP3, Gina M. Lockwood, MD6, Nora G. Kern, MD7, Anne G. Dudley, MD8, Luis H. Braga, MD, PhD5, C. D. Anthony Herndon, MD3, Antoine E. Khoury, MD2, Walid A. Farhat, MD1.
1University of Wisconsin, Madison, WI, USA, 2Children's Hospital of Orange County / University of California, Irvine, Orange, CA, USA, 3Children's Hospital of Richmond at Virginia Commonwealth University, Richmond, VA, USA, 4Children's Hospital of The King's Daughters, Norfolk, VA, USA, 5McMaster University, Hamilton, ON, Canada, 6University of Iowa, Iowa City, IA, USA, 7University of Virginia, Charlottesville, VA, USA, 8Connecticut Children's Medical Center, Hartford, CT, USA.
BACKGROUND: An uncommon congenital anomaly, ureteroceles are challenging to study due to low frequency of presentation. We summarized the clinical characteristics of a large cohort of patients with ureteroceles enrolled in the Societies for Pediatric Urology (SPU) Hydronephrosis Taskforce database. Our objective was to investigate clinical characteristics associated with differences in surgical management among patients diagnosed with ureteroceles.
Methods: We examined patients in the SPU Hydronephrosis Taskforce, which has prospectively enrolled pediatric patients with prenatal hydronephrosis from 7 centers between 2007-2023. We identified patients with ureteroceles, and excluded those with concomitant neurogenic bladder, urethral, and/or genital anomalies. We collected demographic and clinical data including age, gender, circumcision status, ureterocele laterality, duplication, voiding cystourethrogram (VCUG), vesicoureteral reflux (VUR), hydronephrosis, urinary tract infections (UTI) and surgeries performed. We categorized hydronephrosis and VUR using the Society of Fetal Urology (SFU) and International grading systems, respectively. We classified surgeries as early (before 6 months of age) and late (after 6 months of age), and we performed comparative analyses of patients who had early, late, or no surgery. Chi-square or Wilcoxon tests with p-value < 0.05 were considered significant.
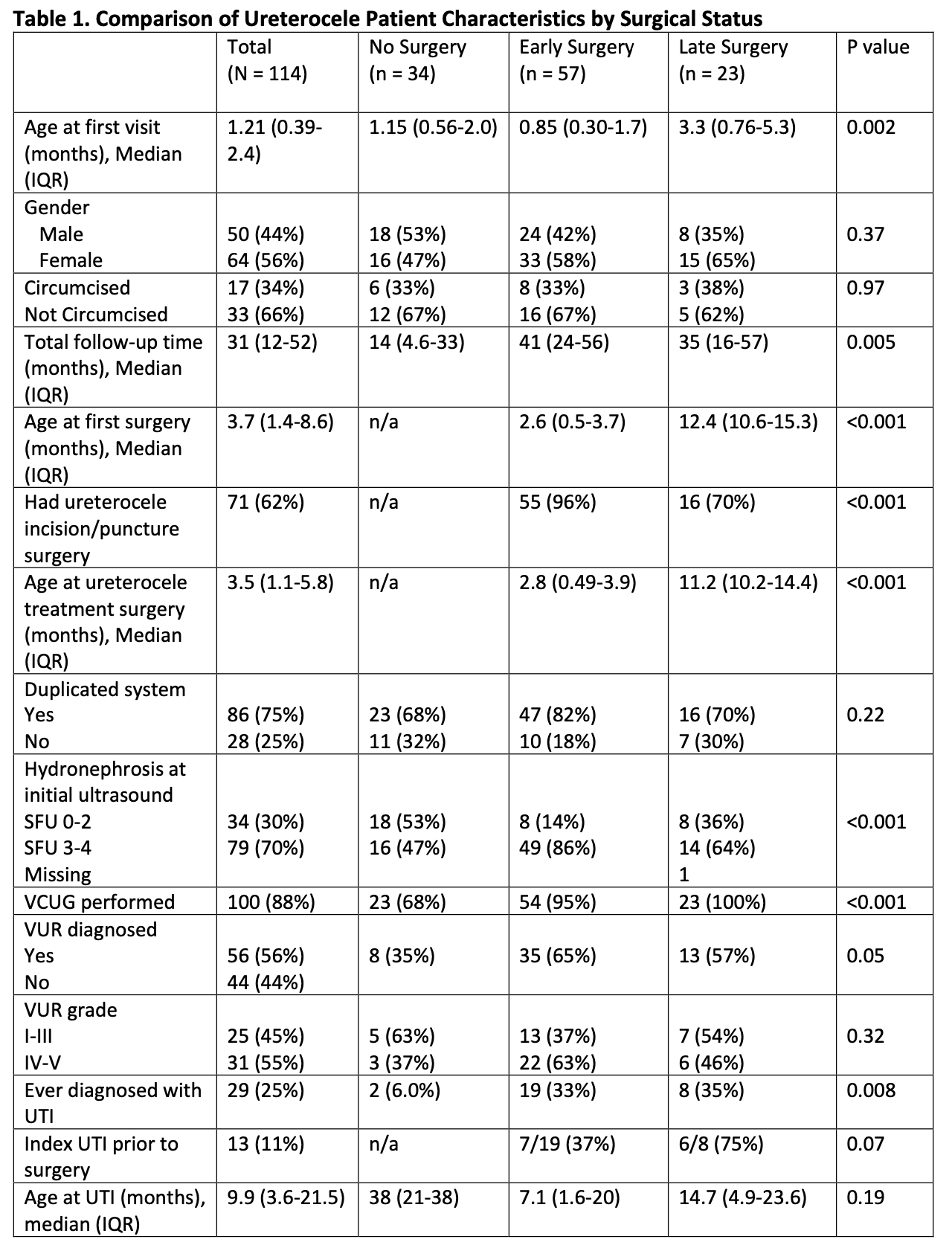
Results: Of 2239 patients in the registry, 114 (5.0 %) had a confirmed ureterocele. Cohort characteristics are outlined in Table 1. Three (2.6%) were bilateral, and 86 (75%) were in a duplicated system. Eighty (70%) patients underwent surgery, of which 57 (50%) were early and 23 (20%) were late. The remaining 34 (30%) did not undergo surgery. Seventy-one (58%) patients underwent ureterocele incision/puncture; most were performed early, and the median time to surgery was 3.4 months (IQR 1.0-5.5 months). Ureteral reimplant was performed in 18 (16%) and median age was 18.1 months (IQR 13.8-20.0 months).
Similar rates of duplicated systems were seen in all groups, including non-surgical patients (p = 0.22). Of those with a VCUG, 56% had VUR. Among children who had surgery, VCUG was performed more often, and VUR was diagnosed with greater frequency (p = 0.05). However, VUR severity did not differ significantly between surgical and non-surgical patients (p = 0.32). While UTIs were more frequent among patients managed with surgery, these UTIs occurred prior to surgery in less than half (13/27 [48%]). Differences in UTI rates between early and late surgery were not statistically significant.
Conclusions: Most ureterocele patients in this large cohort underwent surgical intervention, primarily endoscopic management with puncture or incision. However, almost a third of patients were managed nonoperatively, and most had a duplicated system. While patients who underwent surgery had higher rates of associated VUR and UTIs, VUR severity did not differ from those who did not have surgery and UTIs often occurred after initial surgical intervention. This suggests VUR and UTIs are not driving early decision-making for most. Further study of imaging timing and clinical course are necessary to develop predictive tools for ureterocele management.
Back to 2023 Abstracts
