Association Between Quality of Life and Neurogenic Bowel Symptoms by Bowel Management Program in Emerging Adults with Spina Bifida
N. Valeska Halstead, MD, MPH1, Josephine Hirsch, BA1, Ilina Rosoklija, MA1, James T. Rague, MD1, Soojin Kim, MD2, Theresa Meyer, RN, MS, CPN1, Jill E. Larson, MD1, Vineeta T. Swaroop, MD1, Robin M. Bowman, MD1, Diana K. Bowen, MD1, Stephanie J. Kielb, MD3, Earl Y. Cheng, MD1, Elizabeth B. Yerkes, MD1, David I. Chu, MD, MSCE1.
1Ann & Robert H. Lurie Children's Hospital of Chicago, Chicago, IL, USA, 2BC Children's Hospital, Vancouver, BC, Canada, 3Northwestern Medicine, Chicago, IL, USA.
Background: Neurogenic bowel dysfunction (NBD) is common in spina bifida (SB), with individuals with fecal incontinence (FI) reporting worse quality of life (QOL) compared to those without. Treatment for NBD generally follows a stepwise progression from less-invasive to more-invasive options (e.g., oral medications to enema programs). However, studies assessing the association of bowel management programs and bowel symptoms are limited in scope. We aim to compare differences in bowel-specific QOL, overall QOL, and NBD symptom severity by bowel management program in emerging adults with SB.
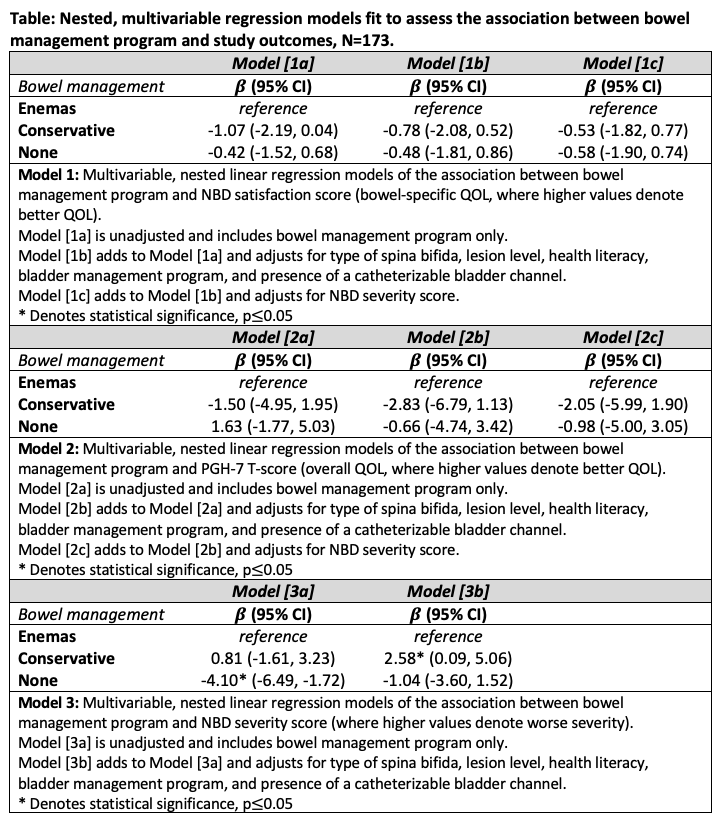
Methods: We performed a retrospective cross-sectional study of patients ≥12 years old at our multidisciplinary SB center from 05/2019 to 02/2020 who completed both a modified Peristeen NBD questionnaire (assessing bowel symptom severity and bowel-specific QOL) and the Patient-Reported Outcomes Measurement Information System Pediatric Global Health questionnaire (assessing overall QOL). Our primary outcomes were NBD symptom severity (scored as a continuous variable), bowel-specific QOL, and overall QOL. Our primary exposure was bowel management program: enemas versus conservative management (e.g. oral medications, manual disimpaction) versus no program. Demographic and clinical characteristics were obtained as covariates from electronic medical record review. Adjusted nested linear and logistic regression models were fit to identify associations between bowel program group and our study outcomes. Two subgroup analyses were performed, stratifying by ambulatory status and myelomeningocele diagnosis.
Results: A total of 173 patients, 56.1% female and 64.6% with myelomeningocele, were included in our analysis. Median age was 18.2 years old (interquartile range 15-21 years old). Patients reported using enemas (n=42), conservative management (n=63), and no bowel program (n=68). After adjusting for covariates, there was no significant association between bowel program and bowel-specific QOL nor overall QOL (see Table). However, the use of conservative management compared to enemas was associated with worse NBD symptom severity (beta=2.58, 95%CI=[0.09,5.06]). Additionally, worse NBD symptom severity was significantly associated with both lower overall QOL (beta=-0.33, 95%CI=[-0.57,-0.10]) and lower bowel-specific QOL (beta=-0.10, 95%CI=[-0.18,-0.02]), even though bowel program itself was not significantly associated with these outcomes. Subgroup analyses by ambulatory status or myelomeningocele diagnosis showed similar null findings for bowel program.
Conclusions: Among emerging adults with SB, NBD symptom severity is more strongly associated with QOL rather than the individual program being utilized or clinical characteristics. Our findings suggest that different degrees of NBD require different invasiveness of bowel programs, but it is the outcome of the bowel management program and not the specific program itself that is most associated with QOL. Bowel management programs and expectations thereof should be tailored to each unique individual with SB.
Back to 2023 Abstracts
