Trends in Door to Detorsion Time in Management of Testicular Torsion: Practice Makes Perfect
Maytal Babajanian, BS1, David Ambinder, MD1, Ryan Lubarsky, BA1, Yuval Elkun, MD2, Henry Dumke, MD3, Joseph Schwob, MD1, Jason Elyaguov, MD4, Miriam Harel, MD5, Paul Zelkovic, MD1, Richard Schlussel, MD1, John L. Phillips, MD1, Lori Dyer, MD1.
1New York Medical College, Valhalla, NY, USA, 2Mount Sinai, New York, NY, USA, 3University of Michigan, Ann Arbor, MI, USA, 4SUNY Upstate, Syracuse, NY, USA, 5Montefiore-Einstein, Bronx, NY, USA.
Background: The management of testicular torsion is a vital and challenging area in pediatric urology. Door to Detorsion time (DTD), a well-known concept in the field, is one of the few factors that can be influenced by both medical providers and institutions. We sought to assess factors that influence door to detorsion time at our institution to provide useful data for clinical decision making and areas of improvement for future management.
Methods: We retrospectively reviewed records of all patients aged 0-18 at our institution with a pre-operative diagnosis of testicular torsion who underwent scrotal exploration from January 2009 to December 2019. Time at ED was defined as time seen by an ED physician. Time at OR was defined as time of arrival into the Operating Room, as recorded in the anesthesia report. We performed linear regression analysis with statistical significance set at a p-value of ≤0.05.
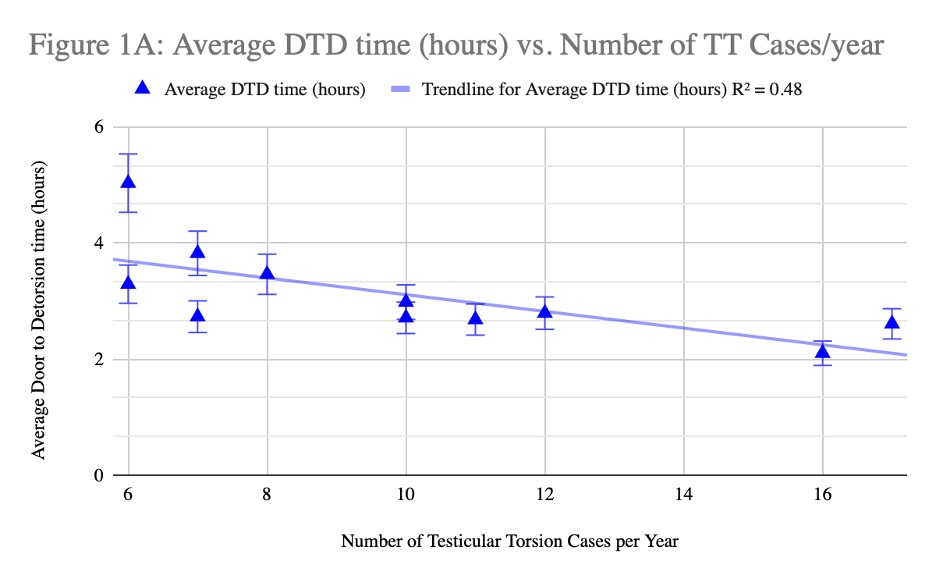
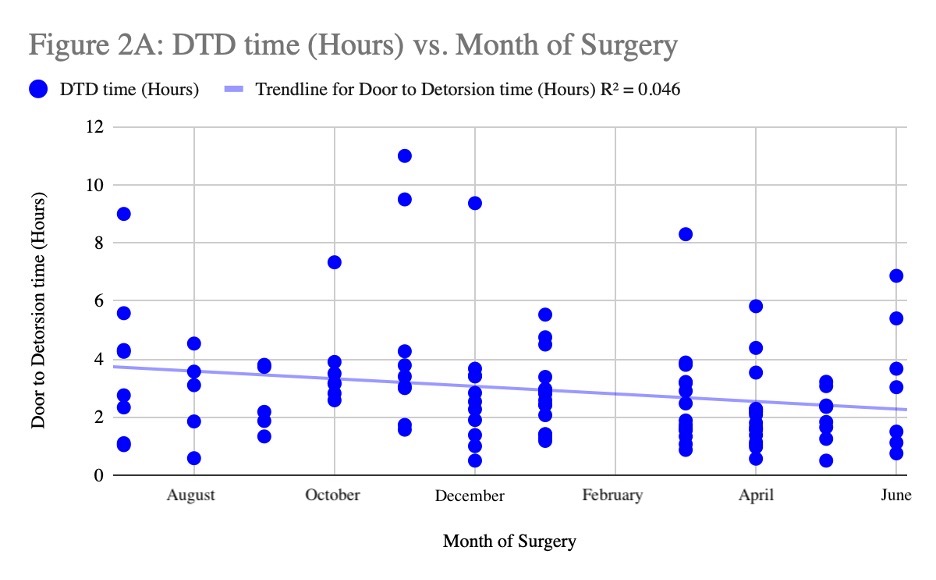
Results: Mean DTD was 2.92 ± 1.96 (hours ± SD). Patients who underwent orchiectomy were associated with a higher DTD of 3.53 ± 2.31 (hours ± SD), vs. 2.71 ± 1.80 (hours ± SD) for orchiopexy (p=.06). Pearson’s correlations demonstrated that the volume of testicular torsion cases was inversely correlated with DTD time (r= -0.69, Figure 1A). Our center improved its ED to OR time over the course of the 11-year period (r= -0.64, Figure 1B). Using the resident academic year as a timeframe, beginning in July and ending in June, we found a mild yet significant decrease in ED to OR time (r = -.21, p=.028).
Conclusion: The DTD time at our institution was inversely correlated with the volume of torsion cases per year, the chronological progression of our institution over 11 years, and across the 12-month resident training and education timeline each year. Our findings suggests that repeated exposure and experience with testicular torsion, both on a resident/medical professional and institutional level, is correlated with shorter DTD times. Further research must be performed to establish a benchmark for a high volume of cases at a center, and to explore alternative training/education avenues for residents at centers with a lower volume of cases.
Figure 1A. Higher volume of testicular torsion cases per year correlates with lower average DTD time (r= -0.69).
Figure 1B. Overall, chronological improvement in DTD time was seen at this institution (r = -.64)
Figure 2A. Composite data from 2009-2019, ordered according to the academic year, ranging from July to June. The data demonstrates that resident training correlates with a lower DTD time (r = -.21, p=.028).

Back to 2023 Abstracts
