OnabotulinumA Toxin Injections: A Novel Option for Management of Refractory Nocturnal Enuresis
Tyler Overholt, MD1, Davis Temple, BS2, Adam Cohen, MD1, Anthony Atala, MD1, Marc Colaco, MD1, Steve Hodges, MD1.
1Atrium Health Wake Forest Baptist, Winston Salem, NC, USA, 2Wake Forest University School of Medicine, Winston Salem, NC, USA.
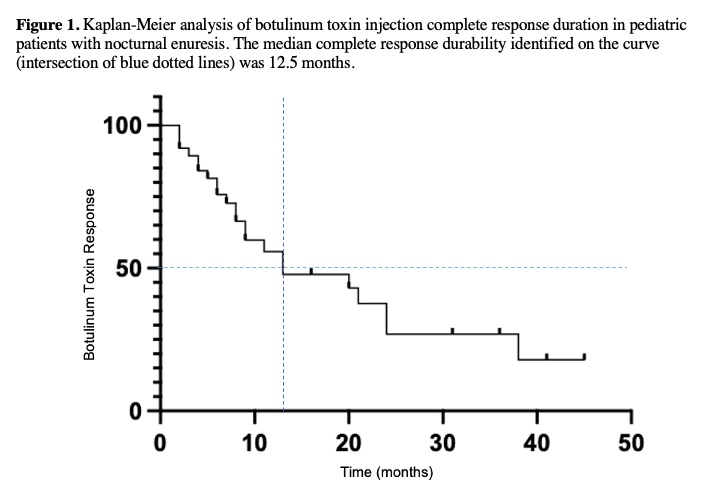
BACKGROUND: The pathophysiology of nocturnal enuresis (NE) is debated within the literature but is thought to be distinct from other voiding disorders. We hypothesize that detrusor overactivity is an underlying driver of this condition. Intravesical OnabotulinumA toxin (Botox) injections are widely utilized for management of symptomatic detrusor overactivity. We sought to assess the efficacy of Botox for management of pediatric patients with NE refractory to multiple lines of therapy. METHODS: We performed a retrospective cohort analysis of pediatric patients who were evaluated at a single tertiary institution for monosymptomatic NE. All patients had nightly incontinence episodes despite previously trialing at least one lifestyle modification (example: alarms), a three-month structured bowel regimen, and at least two medications from different pharmacologic classes (example: Oxybutynin and Desmopressin). Patients with neurogenic diagnoses or any genitourinary abnormality identified on imaging were excluded. The operative procedure was performed per a standardized protocol. Demographic, medical history, and peri-operative data were reviewed. The primary outcome was treatment success, which was defined as complete resolution in incontinent episodes (dryness) or significant improvement in total accident number but without complete resolution. Treatment failure was defined as no improvement in total accident number. We performed descriptive and bivariate statistical analyses as indicated. A Kaplan Meier (KM) analysis was performed to assess failure-free survival. RESULTS: Fifty patients met criteria and were included. The median age was 11 (5-15) years-old, 44% were female gender, and the median operative time was 9 (4-20) minutes. One-hundred units of Botox were administered to 82% and the additional 18% received 200. No intra-operative complications were reported. The median post-procedure follow-up time was 9.5 (2-82) months. Treatment success was observed in 94%, with 58% achieving complete resolution through most recent follow up. There was no difference in improvement (93% vs 100%, p>0.05) or resolution (61% vs 44%, p>0.05) for patients administered 100 vs 200 units. There was also no difference in improvement (93% vs 96%, p>0.05) or resolution (57% vs 59%, p>0.05) in male vs female gender. The median failure free survival identified on KM analysis was 12.5 months (Figure 1). Patients who achieved complete resolution of incontinence following Botox injections were less likely to carry a co-diagnosis of recurrent urinary tract infections (19.4% vs 55.6%, p=0.032), but no association was seen for co-diagnoses of vesicoureteral reflux or encopresis (p>0.05). Five post-operative complications were reported. Four developed a urinary tract infection and one developed retention necessitating a single catheterization.CONCLUSIONS: Intravesical Botox injections were effective for treating NE in 94% of patients with a median failure free survival of 12.5 months. Botox injections were additionally minimally invasive with short operative times and few minor complications in preliminary analyses. Future controlled studies are necessary to further assess this treatment option for refractory NE.
Back to 2023 Abstracts
