Novel use of a commercial enuresis alarm to detect voiding in hospitalized infants: a pilot study to determine safety and feasibility
Peter Y. Cai, MD, Andrea Balthazar, MD MPH, Regina L. Tham, BS, Badar Omar, BA, Bartley G. Cilento, Jr., MD MPH, Caleb P. Nelson, MD MPH.
Boston Children's Hospital, Boston, MA, USA.
BACKGROUND: An essential step in evaluating bladder function is documentation of complete bladder emptying by measuring post-void residual (PVR) by ultrasound or catheterization immediately after voiding. In non-toilet trained, non-verbal patients (such as infants or patients with severe neurological impairments), accurate determination of timing of voiding can be challenging. This leads to inaccurate PVR measurements since the PVR is not assessed immediately after voiding. Enuresis alarms are triggered by moisture, raising the possibility of using them to indicate voiding in patients otherwise unable to indicate that voiding has occurred. In this pilot study, we sought to test the practicality, feasibility, and safety of using an enuresis alarm to indicate voiding in hospitalized infants. We hypothesized that this device can be used in a novel manner to reliably determine timing of voiding.
Methods: After obtaining institutional review board approval and parental consent, we prospectively enrolled ten infants between October 2022 and April 2023 in our neonatal intensive care unit (NICU). Inclusion criteria were: (1) adjusted post-conceptual age between 36 and 50 weeks and (2) hospitalization for non-surgical management of feeding issues or respiratory concerns. Exclusion criteria were: (1) known urological or neurological conditions, (2) urinary tract infection, or (3) indwelling urinary catheter. A four-hour study period was conducted where the enuresis alarm was placed inside the diaper and diaper status (wetness, color indicator change) was noted with each alarm activation. Diaper was inspected at regular intervals (15 to 30 minutes) during the study period to capture any voids not detected by the alarm. The primary endpoints for this pilot study were correlation of alarm activation with voids (wet diapers) and incidence of technical difficulties.
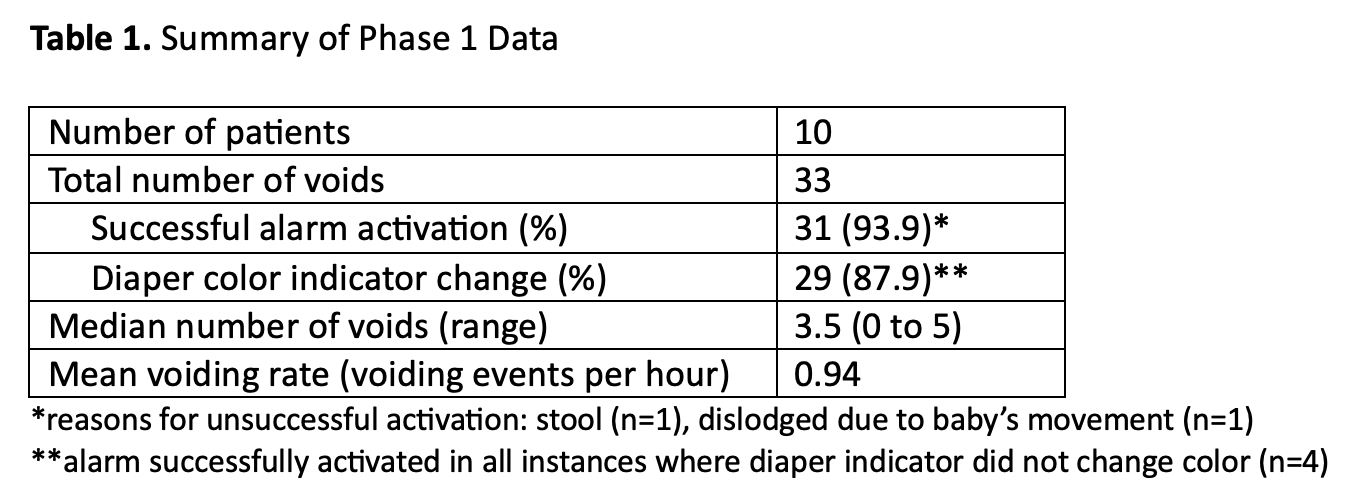
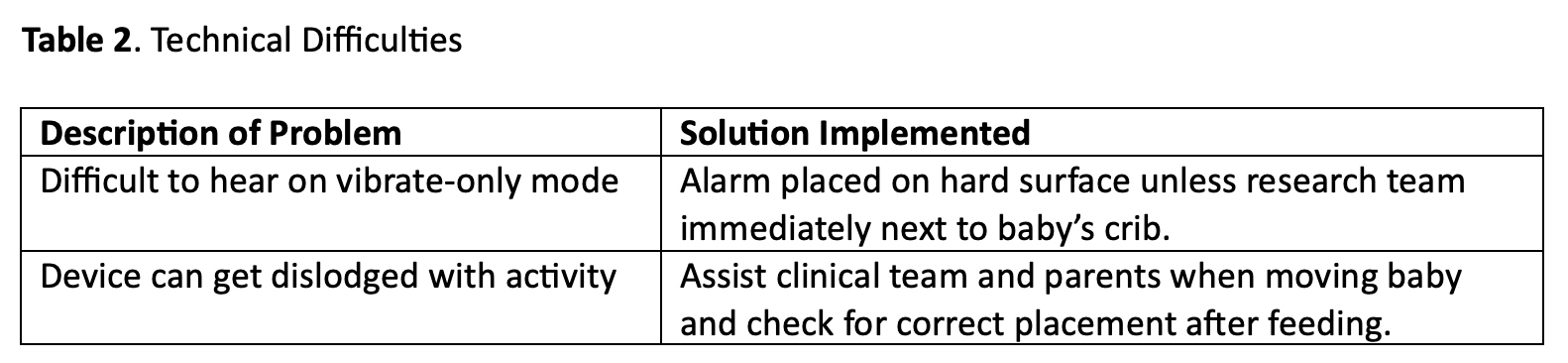
Results: Median weight was 4.14 kg (range 2.46 to 6.70 kg) and median length was 51 cm (range 45 to 61 cm). Reasons for NICU admission were respiratory syncytial virus bronchiolitis (n=5), supraventricular tachycardia (n=1), hypoglycemia (n=1), respiratory failure (n=1), apnea (n=1), and feeding evaluation (n=1). Across all infants, 33 total voids were captured during the study period with a median of 3.5 voids per infant (Table 1). We found that the enuresis alarm successfully activated in 31 of 33 voids (93.9%). Of the 33 voids, the external diaper indicator changed color in 29 (87.9%). Technical difficulties were uncommon (Table 2). No adverse events occurred and no concerns regarding clinical workflow were reported by nursing during the study periods.
Conclusions: A commercially available enuresis alarm detected more than 90% of voids in a cohort of NICU infants in a time-sensitive manner with no feasibility or safety concerns. This novel use for the enuresis alarm is promising and further studies should evaluate its potential role in determining PVR in patients for whom accurate measurement of bladder emptying is important.
Back to 2023 Abstracts
