Who knows when the ball should drop? A survey study of pediatric primary care providers and trainees on management of undescended testes
Amanda Raines, MD, Paul Merguerian, MD, Mark Cain, MD, Nicolas Fernandez, MD, Byron Joyner, MD, Kathleen Kieran, MD, Margarett Shnorhavorian, MD, Jennifer Ahn, MD.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: Despite the American Urologic Association (AUA)'s 2014 guideline update regarding the management of undescended testes (UDT), the average age of orchiopexy remains above that in the recommendations. To better understand potential barriers to timely orchiopexy, we aimed to assess current practice patterns of pediatric primary care providers (PCPs) and trainees in the management of undescended testicles utilizing an online survey. We hypothesized that some providers would not be adherent to guidelines and the trainee education on UDT would be limited. Methods: After obtaining IRB approval, we developed and distributed a brief, anonymous survey to pediatric PCPs in Washington state with questions focused on their management of UDT. A separate survey was distributed to pediatric and family medicine residents focused on their educational experience and understanding of UDT management. Pediatricians were identified using the American Academy of Pediatrics (AAP) directory and emailed directly. Family medicine physicians and advance practice providers were provided the survey request via their respective Washington state chapter national organizationís newsletters. Pediatric and family medicine trainees in residency programs in California, Oregon, and Washington were included. The survey was distributed to program directors or coordinators who were requested to disperse the survey to their trainees.
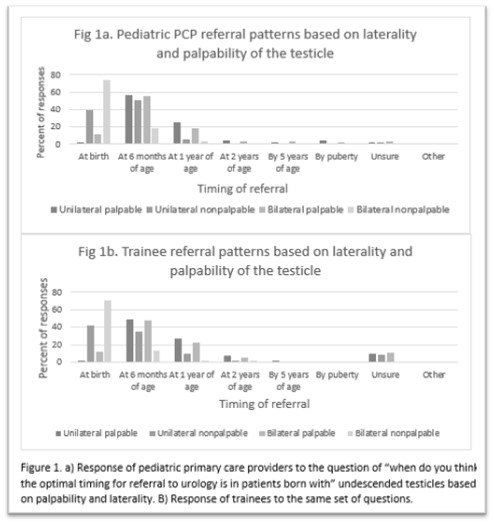
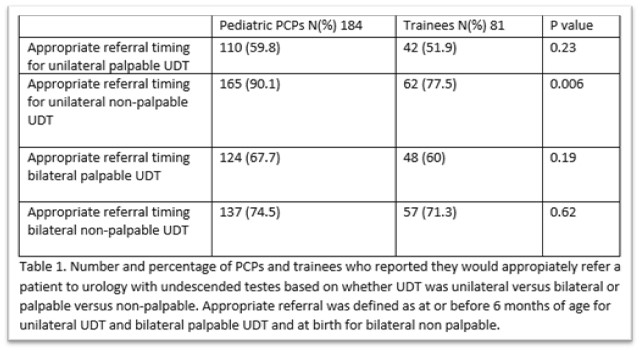
Results: A total of 184 pediatric PCPs and 81 trainees completed the survey. The response rate of pediatricians, who made up 87% of respondents, was 15.5%, while that of family medicine providers was 0.1%, likely due to the inability to contact the providers directly by e-mail. Regarding timing of referral, the majority of PCPs (75%) and trainees (71%) appropriately reported referring at birth for bilateral nonpalpable testes (Fig 1). However, 48% of trainees reported late referral (>1 year of age) for unilateral palpable UDT (Table 1). When asked scenarios in which participants would order an ultrasound prior to referral to urology, 40% of pediatric PCPs and 47% of trainees reported ordering ultrasounds for non-palpable testes. Twenty three percent of trainees reported ordering ultrasounds on all patients, while only 7.4% stated they would never order an ultrasound. Thirty five percent of trainees reported no educational experiences on managing UDT during training. Half of trainees reported never being trained on examination techniques for UDT. Conclusions:
While this survey showed improvements in reported timing of referral for UDT compared to prior ones, there is still room for improvement particularly in palpable UDT. Additionally, efforts should be focused on ultrasound guidelines and trainee education. Response rates were limited by distribution means in all groups except for pediatricians who were directly emailed and had the highest response rate which was similar to prior studies.
Back to 2023 Abstracts
