Reducing disparities in access to ambulatory pediatric urologic care: Development and assessment of an outbound scheduling intervention
Jennifer Ahn, MD, MS.
Seattle Children's Hospital, Seattle, WA, USA.
BACKGROUND: The majority of pediatric urology is provided in the ambulatory setting, with clinic visits playing an essential role in evaluation and maangement. Missed clinic visits can negatively impact patients, providers, and the health system, and are often associated with social determinants of health (SDOH). The aims of this study were 1) to evaluate the proportion of missed visits and associated factors, 2) implement an intervention designed to reduce missed visits, and 3) assess the impact of intervention on missed visits.
Methods: The pediatric urology ambulatory visits at a tertiary care hospital and its regional clinics were evaluated over a 6 month pre-intervention period (September 2022 to February 2023). The total number of visits were evaluated and determined to be completed or missed (e.g. no-shows). Patient sociodemographic and clinical characteristics were assessed, as were clinic site, provider, provider type, and visit type. During this pre-intervention phase, caregivers/patients received the standard phone and text reminders of the upcoming appointments. The pre-intervention data were analyzed and a predictive model was created using 21 factors. During the intervention phase (March 2023-present), upcoming visits that were high-risk of being missed based on the model were targeted with outbound care calls. During this call, information was provided, questions were addressed, and potential barriers were assessed with help offered as needed, such as transportation or childcare support. The intervention phase data were assessed regarding missed visits and success of outbound care calls. Chi-square and logistic regression analyses were performed using Stata.
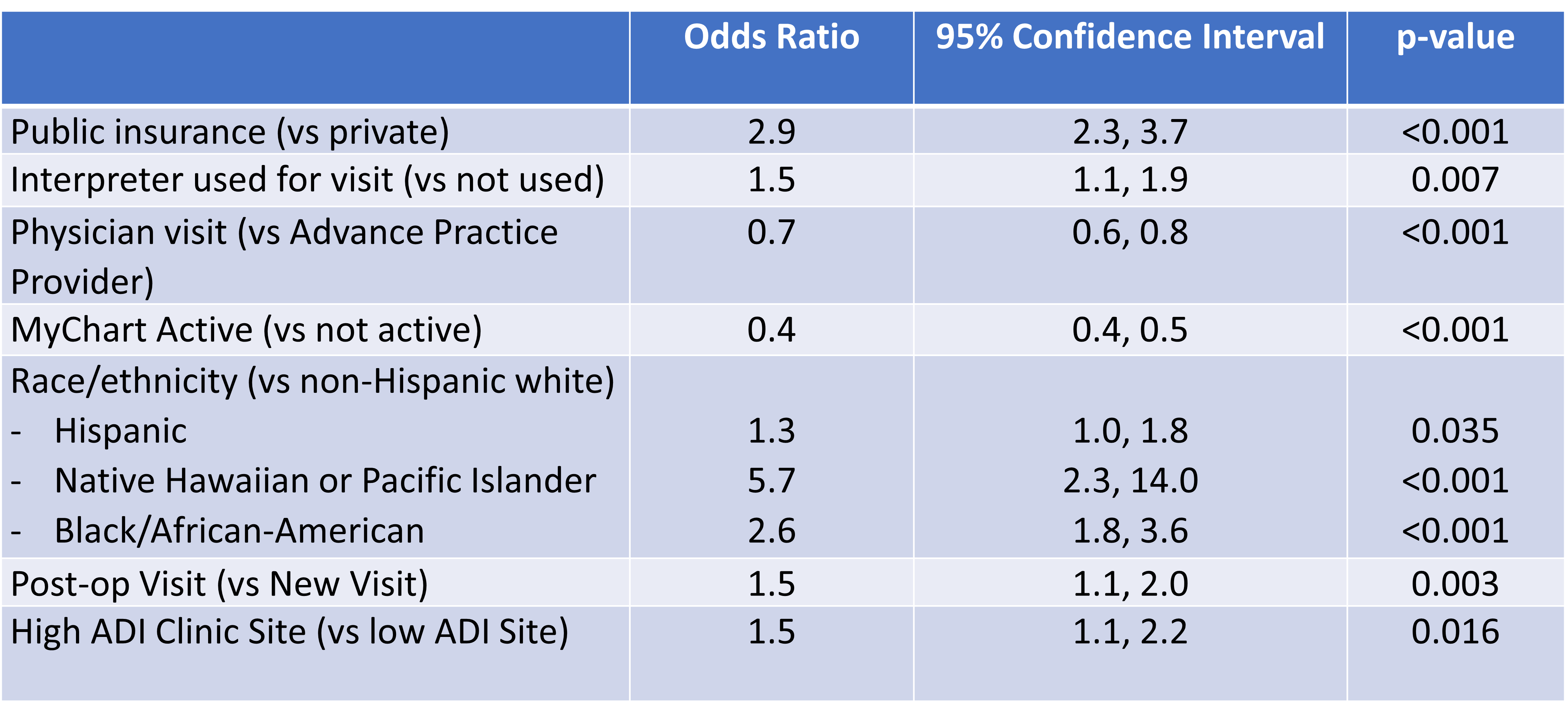
Results: During the pre-intervention phase, there were 5902 total visits, 556 (9.4%) of which were missed. Missed visits were associated with clinic location, with higher rates (15.4%) seen in areas with higher Area Deprivation Index (ADI) compared with clinics in low ADI locations (6.6%), p <0.001. Missed visits were associated with race and ethnicity, with highest rates seen amongst Black and African American patients and Native American and American Indian on univariate and multivariate analysis (p<0.001). Interpreter use and public insurance were also associated with higher likelihood of missed visits (p <0.001). Active my chart status, visit with physician (versus advanced practice provider), and telehealth visit were all associated with lower likelihood of a missed visit (Table 1). During the first 2.5 months of intervention, 184 visits were identified as >50% likelihood of being missed and were targeted with an outbound care call. 78% (143) of those visits were completed, 11% (21) were canceled, with 6/21 (29%) canceled spots filled. The overall missed visit rate was 7.9%, representing a 17% reduction in missed visits compared with pre-intervention.
Conclusions: SDOH are associated with increased likelihood of missed ambulatory visits. A targeted, data-driven intervention can improve equitable access to care.
Back to 2023 Abstracts
