Perioperative Opioids Prescribing Following Pediatric Urology Procedures is Associated With Persistent Opioid Use Disorder - A Large Claims Database Analysis
Aurora Grutman, BS1, Courtney Stewart, BA2, Pranjal Agrawal, BA1, Corey Able, BS3, Logan Galansky, MD4, Andrew Gabrielson, MD4, Nora Haney, MD4, Taylor P. Kohn, MD, MPhil4, Chad B. Crigger, MD4.
1Johns Hopkins University School of Medicine, Baltimore, MD, USA, 2University of Texas Medical Branch School of Medicine, Galveston, TX, USA, 3University of Texas Medical Branch Department of Surgery, Division of Urology, Galveston, TX, USA, 4The James Buchanan Brady Urological Institute, Johns Hopkins University School of Medicine, Baltimore, MD, USA.
BACKGROUND: Pain management practices involving perioperative opioid use have contributed to a nationwide opioid epidemic. This study aimed to assess the risk of persistent opioid use associated with various pediatric urologic procedures.
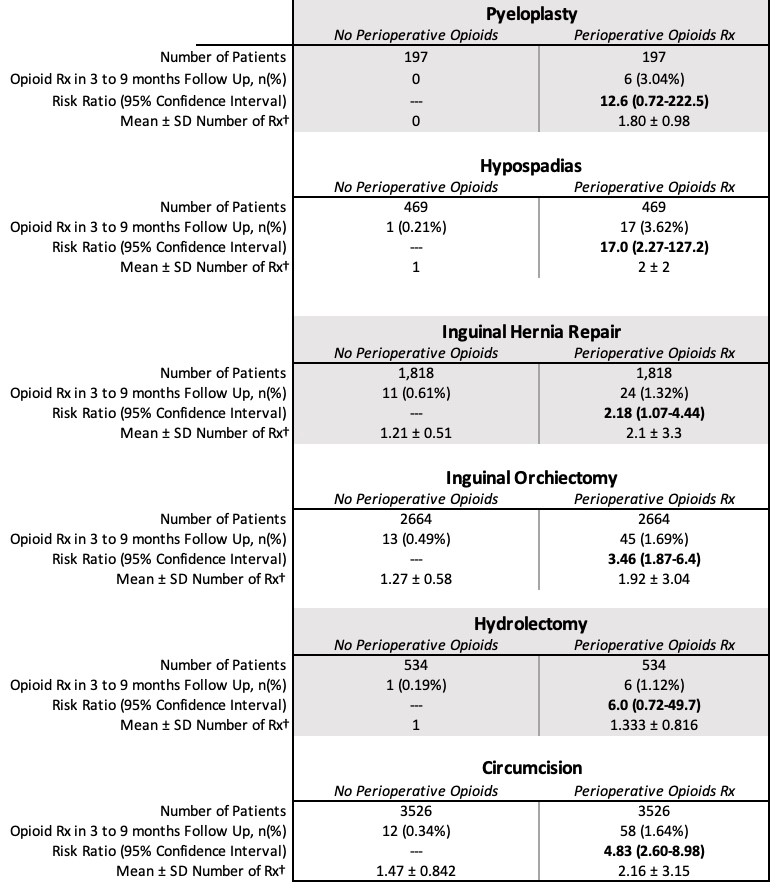
Methods: The TriNetX LLC Diamond Network was queried for adolescents aged 13 to 21 years who underwent six urologic procedures (pyeloplasty, hypospadias repair, inguinal hernia repair, inguinal orchiectomy, hydrocelectomy, or circumcision) and created cohorts of patients who were or were not prescribed postoperative opioids. Propensity matched scoring was performed for age, race/ethnicity, psychiatric diagnoses, and preoperative pain diagnoses. The primary outcome was new persistent opioid use, defined as new opioid use 3-9 months after index procedure without another ED visit or surgery during that timeframe.
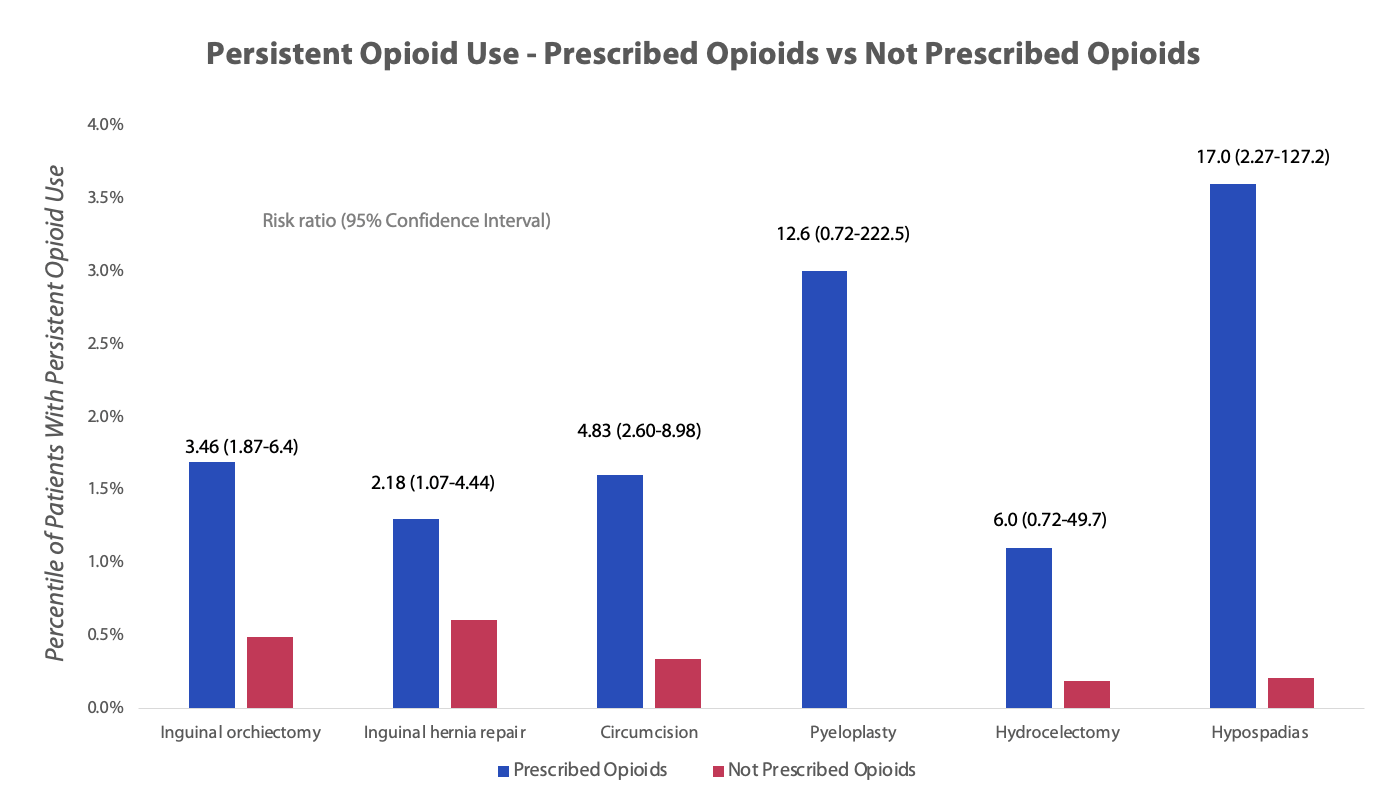
Results: Overall, we identified 32,789 adolescents of which 66.0% received a perioperative opioid prescription. After propensity score matching, 18, 416 patients were included: 197 for pyeloplasty, 469 for hypospadias repair, 1,818 for inguinal hernia repair, 2,664 for inguinal orchiectomy, 534 for hydrocelectomy, and 3,526 for circumcision. Overall, 0.41% of patients who did not receive perioperative opioids developed new persistent opioid use, whereas 1.69% of patients who received perioperative opioids developed new persistent opioid use (p<0.05). Patients who received perioperative opioids had statistically higher odds of developing new persistent opioid use after hypospadias repair (Risk Ratio (RR): 17.0; 95% Confidence Interval (CI): 2.27-127.2), inguinal orchiectomy (RR: 3.46; 95% CI: 1.87-6.4), inguinal hernia repair (RR: 2.18; 95% CI: 1.07-4.44), and surgical circumcision (RR: 4.83; 95% CI: 2.60-8.98). There was no significant risk of developing new persistent opioid use with a prescription of perioperative opioids following pyeloplasty or hydrocelectomy.
Conclusions: We found that the use of perioperative opioids in several pediatric urological procedures is associated with a significant risk of developing new persistent opioid use.
Back to 2023 Abstracts
