Opioid Prescribing Patterns and the Effect of Chronic Kidney Disease in Pediatric Urology Population: A Retrospective Cohort Analysis
Kristen Meier, MD1, Darren Ha, MS2, Eliza Blanchette, MD1, Megan Brockel, MD1, Vijaya Vemulakonda, JD, MD1, Kyle Rove, MD1.
1Children's Hospital Colorado, AURORA, CO, USA, 2University of Colorado School of Medicine, AURORA, CO, USA.
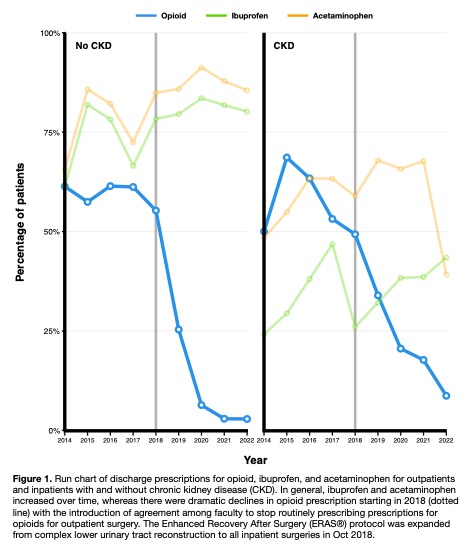
BACKGROUND: Significant efforts have been undertaken to decrease opioid prescribing, but there is little research into patient-specific factors presenting as barriers in the pediatric surgical population. We implemented an Enhanced Recovery After Surgery (ERAS) protocol in pediatric urology in 2014, expanded it in 2018, and stopped routinely prescribing opioids after outpatient surgery in 2019. Minimizing opioids is an important ERAS tenant, but data is limited on the interplay of chronic kidney disease (CKD) on opioid prescribing. We hypothesized that opioid reduction efforts were successful, but patients with CKD would be more likely to receive an opioid prescription than those without CKD.
Methods: A retrospective cohort study of patients ≤18 years old undergoing urologic surgery from 2014-2022 was performed. Patients were stratified by CKD diagnosis. CKD was determined by a diagnosis in the chart and confirmed with the CKiD U25 eGFR calculations using most recent preoperative lab values. Only laboratory-confirmed, abnormal GFR values were considered CKD for the purposes of this study. Patients were propensity matched on variables such as admission class, sex, race, insurance, surgeon, year of surgery, comorbidities, operative time, and prior opioid exposure using the optimal full algorithm. Outcomes of interest were opioid prescriptions at discharge, non-opioid analgesic prescriptions, and unscheduled postoperative healthcare encounters (emergency department visits, readmissions, or reoperations within 30 days).
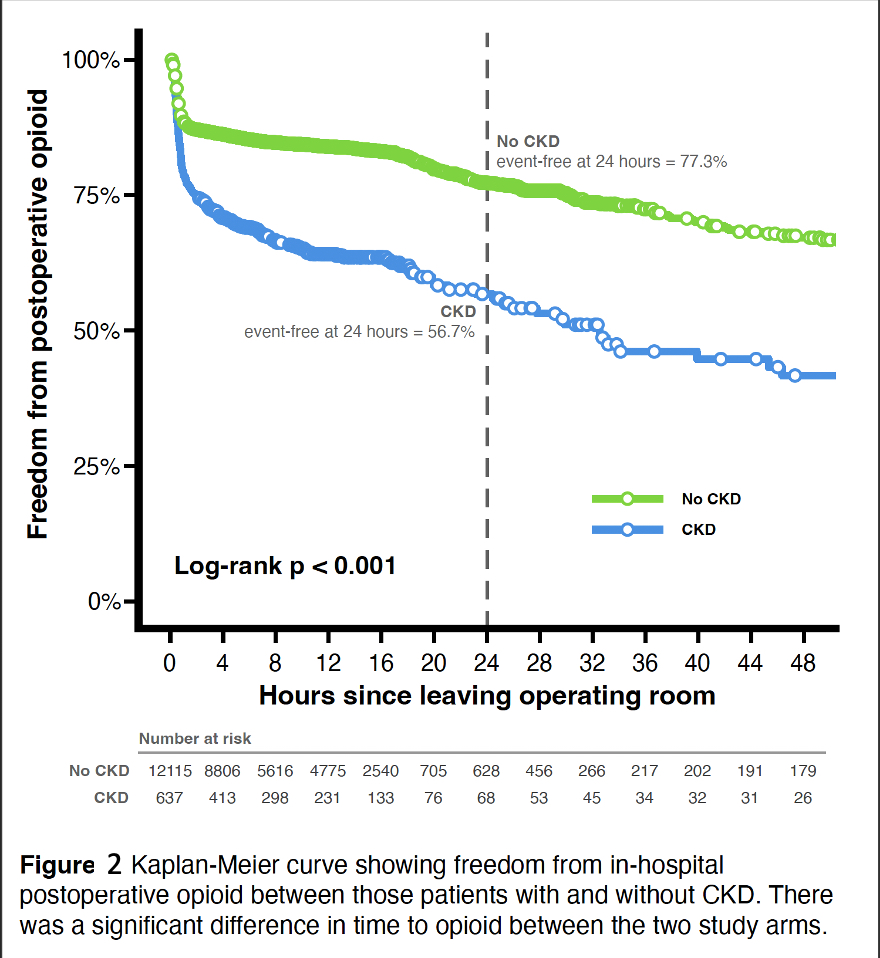
Results: 12,752 patients were included. 637 patients (5.0%) had a pre-existing CKD diagnosis; the majority were CKD stage 2 (75.4%, 477 patients). A significant decrease in discharge opioid prescriptions was seen for patients with and without CKD (Figure 1). CKD patients had greater opioid exposure prior to surgery, although this was not statistically significant (18.2%, 116 vs 3.2%, 383, p=0.09). Kaplan-Meier analysis demonstrated a significantly shorter time to first in-hospital postoperative opioid administration in those with CKD (p<0.001)(Figure 2). Unsurprisingly, CKD patients were less likely to receive NSAIDs (p<0.001), although opioids were equally likely to be prescribed at discharge (p=0.62). Patients with CKD were more likely to present to the emergency department (ED) within 30 days of surgery (17.7% vs 11.2%, p<0.001).
Conclusions: Multiple interventions and a dedicated postoperative opioid reduction protocol worked well, even for the subset of patients with CKD where there is concern regarding the safety of NSAID use. While similar proportions of CKD and non-CKD patients received an opioid prescription at discharge, patients with CKD were more likely to have earlier postoperative, in-hospital opioid exposure and present to the ED within 30 days of surgery. In efforts to improve outcomes, additional work is necessary to identify barriers and optimize protocols for patients with CKD.
Back to 2023 Abstracts
