A single-institution prospective cohort study of assisted bladder emptying following primary cloacal repairs performed between 2020 - 2021
Meghan Davis, MD, MPH, Shruthi Mohan, BA, Teresa Russell, MS, Christina Feng, MD, Andrea Badillo, MD, Marc Levitt, MD, Christina P. Ho, MD, Hans G. Pohl, MD, Briony K. Varda, MD, MPH.
Children's National, Washington, DC, USA.
Background
Although the combination of bladder dysfunction and upper tract anomalies puts patient with cloaca at risk for renal disease, the rarity of this condition makes it difficult to study empirically. As a high-volume center, we uniquely capture bladder function outcomes following our growing number of cloacal repairs.
Objective
1) Describe the rates of incomplete bladder emptying following primary cloacal repair (at 2-3 months after repair and last follow up visit), and 2) identify clinical factors associated with assisted bladder emptying.
Study Design
We performed a prospective cohort study of patients undergoing primary cloaca repair our institution’s Colorectal Center team between 2020 and 2021. The primary outcome was assisted bladder emptying at 2-3 months postoperatively and last visit. Covariables included cloacogram measurements (urethral length, common channel length), vesicoureteral reflux (VUR) status, sacral ratio (good ≥0.7, intermediate 0.7 – 0.4, poor ≤0.4), spinal cord status (low conus/tethered cord, fatty filum, caudal regression), assisted bladder emptying preoperatively, and operative details (age at repair, repair type, & concomitant laparotomy). Unadjusted descriptive statistics were performed.
Results
Eighteen participants were eligible. A majority had moderate cloaca (78%), VUR (67%), spinal cord abnormalities (89%), and good sacral ratios (56%). Preoperatively, 10 patients were diapered for urine and 8 had assisted bladder emptying. Surgical repairs were performed at a median age of 8 months (range 4 – 46). Nine (50%) patients underwent urogenital separation (UGS), eight (44%) total urogenital mobilization, and 1 (6%) perineal sparing posterior sagittal anorectoplasty with introitoplasty. Exploratory laparotomy was performed in 7 (39%).
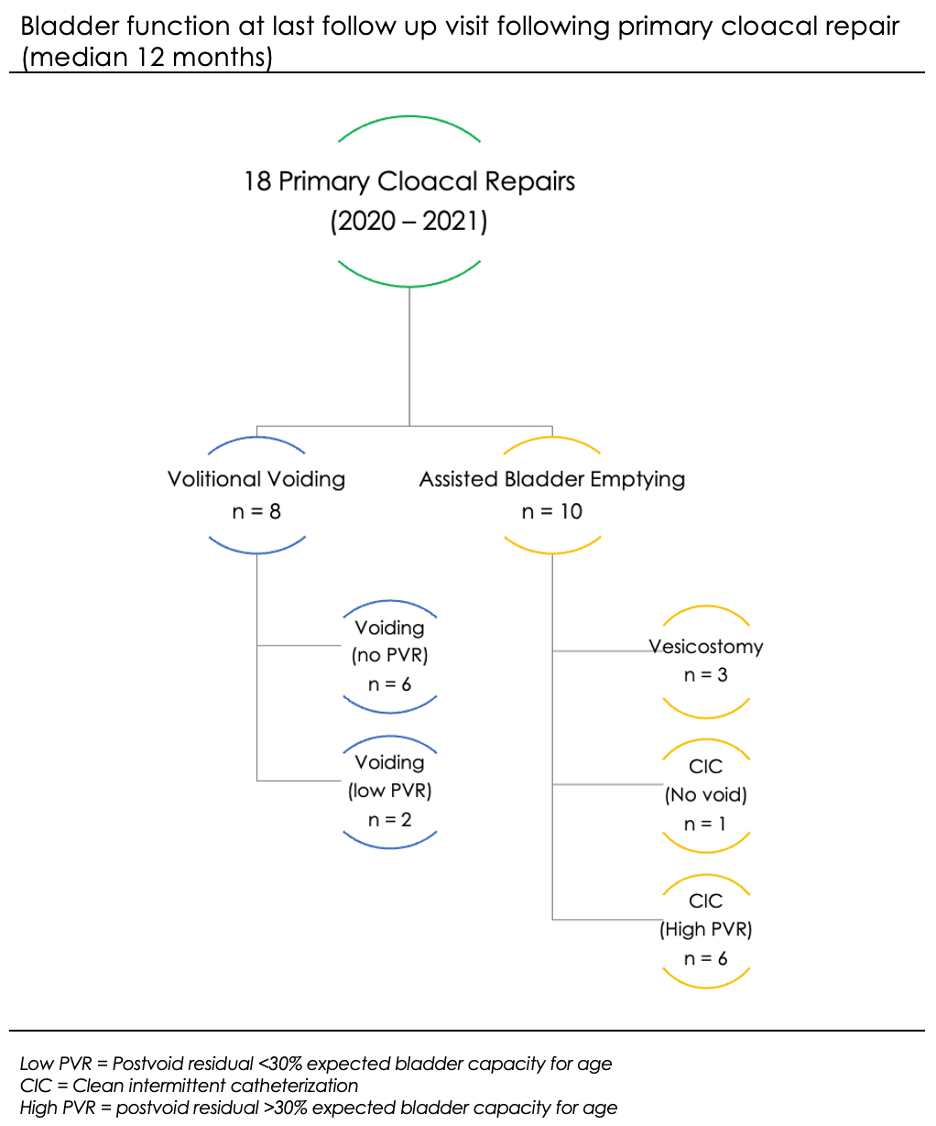
At 2-3 months after repair, 7 patients were voiding and 11 required assisted bladder emptying. The median time to last visit was 12 months (range 5 – 25), at which point 8 patients were voiding and 10 required assisted bladder emptying. In unadjusted analysis, postoperative need for assisted bladder emptying was significantly associated with assisted bladder emptying preoperatively (e.g. vaginostomy or CIC), a shorter urethra (≤1.8-cm) and increasing common channel length (≥2.9-cm), UGS (vs. other surgical approaches) and exploratory laparotomy (p<0.05 for all). Spinal cord imaging findings were not associated (p = 0.7).
Conclusion
Approximately half of patients required assisted bladder emptying in this study. Associated factors included shorter urethral and a longer common channel lengths, the need for assisted bladder emptying preoperatively, the type of surgical approach (namely UGS) and additional laparotomy. Being diapered with seemingly normal voiding prior to surgery did not guarantee normal bladder function postoperatively. In some patients, immediate postoperative bladder function may change with time.
Back to 2023 Abstracts
