What’s the point of pyuria? Rethinking the threshold for a significant urinary white blood cell count for urinary tract infection among children with spina bifida
Victor Kucherov, MD, Teresa L. Russell, MS, Jacob C. Smith, MD, Sally K. Zimmermann, BA, Elena K. Johnston, BS, Md Sohel Rana, MBBS, MPH, Elaise Hill, MD, Christina P. Ho, MD, Hans G. Pohl, MD, Briony K. Varda, MD, MPH.
Children's National Hospital, Washington, DC, USA.
BACKGROUND: Pyuria defined as >10 WBC/HPF is a core component of spina bifida specific criteria for urinary tract infection (UTI), however this threshold is largely historical and may not ideally classify those with symptomatic infection. The study aims to identify a more optimal threshold for “significant” pyuria, defined as one which maximizes the area under the receiver-operator curve (AUC) with respect to identifying patients with true symptomatic infection.
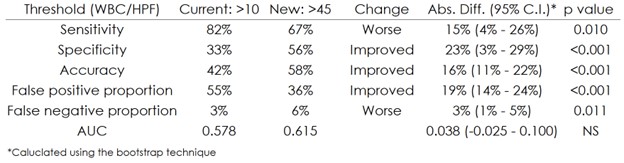
Methods: A retrospective review of children with spina bifida (age < 21) evaluated in the emergency department (ED) was performed. Patients with a urinalysis (UA) and urine culture who were reliant on assisted bladder emptying (e.g., intermittent catheterization) were included. The primary outcome was symptomatic bacteriuria, defined as ≥ 2 urologic symptoms (fever ≥38 C, black/flank pain, abdominal pain, pain with catheterization, new/worsened urinary incontinence, and malodorous/cloudy urine) with >100k CFU urine culture. The primary exposure was WBC/HPF on UA. Sensitivity analysis was performed to identify an optimal WBC/HPF threshold to maximize the AUC with respect to correct classification of patients with symptomatic bacteriuria. Descriptive statistics were performed in addition to test characteristics based on this threshold, including its sensitivity, specificity, accuracy, and the percentage of all patients classified as false positives and false negatives. The 95% confidence intervals (CI) for differences between test characteristics were calculated to assess for statistical significance.
Results: Out of 809 ED encounters queried, a total of 225 were identified for inclusion. The median WBC/HPF identified was 40 (range 0 - 3,607) with 70% of patients having >10 WBC/HPF. Symptomatic bacteriuria was identified in 17% of patients. Test characteristics for the current >10 WBC/HPF threshold are shown in the Table, including sensitivity, specificity, accuracy, the proportion of the total cohort that were false positives/negatives, and AUC. Following sensitivity analysis, a new threshold of >45 WBC/HPF was identified which maximized the AUC (0.615). This threshold of >45 WBC/HPF was identified in 48% of patients. Compared to >10 WBC/HPF, the >45 WBC/HPF threshold produced statistically significant improvements in specificity, accuracy, and false positive proportion of the cohort, but worsened sensitivity and the false negative proportion of the cohort (Table). Even after optimization however there was no statistically significant difference in model AUC.CONCLUSIONS: Compared to the current threshold of >10 WBC/HPF (which was no better than a coin flip), pyuria redefined to >45 WBC/HPF significantly improved the accuracy of identifying symptomatic infection. However, even at this optimized value the overall model performance remained poor, calling into question pyuria’s added value (at any threshold) to UTI diagnosis for this population.
Back to 2023 Abstracts
